Psoriasis isn’t just a skin condition-it’s your immune system going haywire. Thick, scaly patches show up not because your skin is dirty or broken, but because your body is attacking itself. And while genetics lay the groundwork, it’s the triggers-stress, infections, and damaged skin-that turn up the volume on those flares. If you’ve ever watched a mild patch explode into something painful and widespread after a bad week at work or a bad cold, you’re not imagining it. There’s science behind why that happens.
Stress Doesn’t Just Feel Bad-It Makes Psoriasis Worse
Stress is the number one trigger reported by people living with psoriasis. It’s not just about feeling overwhelmed. When your body is under stress-whether from grief, a new job, or even a vacation-it releases cortisol and other inflammatory chemicals. These don’t just make you feel tense; they wake up immune cells in your skin that shouldn’t be active.
Research shows that stress directly disrupts the skin’s natural barrier. That means more moisture escapes, your skin gets drier, and irritants slip in more easily. A 2024 study in JAMA Dermatology confirmed this: psychological stress breaks down the skin’s protective layer, making it easier for inflammation to take hold.
And here’s the cruel twist: having psoriasis causes stress, which then makes psoriasis worse. It’s a loop. One Reddit user shared that after losing their mother, their psoriasis went from small elbow patches to covering 30% of their body in three months. That’s not rare. Studies show that 70% of patients link their worst flares to major emotional events.
Breaking the cycle doesn’t mean eliminating stress-it means managing it. Daily mindfulness meditation for just 20 minutes can drop cortisol levels by 25% in eight weeks. Regular walking, therapy, or even journaling can help. One dermatology practice tracked patients who practiced mindfulness for six months and found 67% had at least a 30% drop in flare frequency.
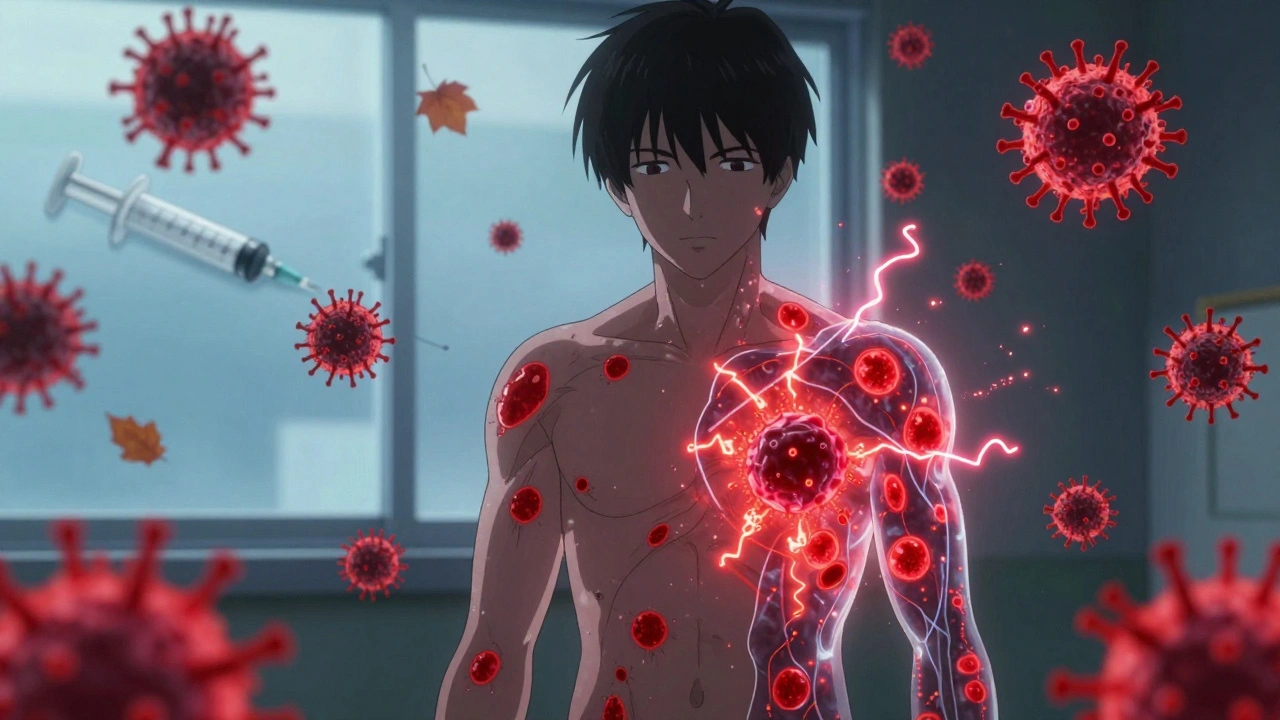
Infections Are Silent Spark Plugs for Flares
Think of infections as a match to your psoriasis gasoline. A sore throat, the flu, or even COVID-19 can trigger a sudden outbreak-especially in younger people. Streptococcal infections, like strep throat, are the most common culprits behind guttate psoriasis, a type that looks like small, drop-like spots all over the torso and limbs.
Here’s how it works: when your body fights off a virus or bacteria, it activates immune sensors called RIG-I. In people genetically prone to psoriasis, this triggers a chain reaction that releases IL-23, a powerful inflammatory signal. That signal tells skin cells to multiply too fast-and boom, plaques appear.
Even HIV, which wipes out immune cells, can worsen psoriasis. That’s because the immune system becomes chaotic, not just weak. The body overcompensates, and inflammation spikes.
Prevention is simple but powerful: wash your hands often, get your flu shot, and treat infections early. One study found that people who got their annual flu vaccine had 35% fewer infection-triggered flares. Don’t wait until you’re sick to act. Vaccines and hygiene aren’t just for kids-they’re part of your psoriasis management plan.
Your Skin Barrier Is Your First Line of Defense
Psoriasis doesn’t start in the bloodstream-it starts in the skin. When the outer layer gets damaged, whether by scratching, sunburn, insect bites, or harsh soaps, your immune system responds as if there’s an injury. That’s called the Koebner effect. Up to 45% of new plaques form exactly where the skin was injured, even if the injury seemed tiny.
That’s why skin barrier care isn’t optional-it’s essential. Your skin’s barrier is made of lipids, proteins, and natural moisturizing factors. When you use scented soaps, hot showers, or alcohol-based cleansers, you strip those away. The result? Dry, cracked skin that invites bacteria and triggers inflammation.
The American Academy of Dermatology recommends three simple steps: use fragrance-free moisturizers with ceramides twice a day, keep indoor humidity between 40% and 60%, and avoid soaps with a pH higher than 5.5. Ceramides are the glue that holds skin cells together. Replenishing them helps stop the cycle of damage and flare.
Studies on mice with damaged skin barriers showed that applying topical antibiotics reduced psoriasis-like symptoms by cutting down harmful bacteria and lowering IL-17 and IL-22, two key inflammatory drivers. While you won’t use antibiotics daily, this proves that keeping your skin’s microbiome balanced matters.

What You Can Do Right Now
You don’t need to overhaul your life to control flares. Start with three small, doable changes:
- Moisturize daily. Apply a thick, fragrance-free cream or ointment within three minutes of showering. Look for ceramides, hyaluronic acid, or colloidal oatmeal.
- Track your triggers. Use a simple notebook or phone app to log stress levels, illnesses, and new skin changes. Over time, patterns emerge. One patient found 78% of their flares followed either stress or infection.
- Protect your skin. Wear gloves in cold weather, use insect repellent, avoid scratching, and treat sunburns immediately. Even a minor scrape can spark a new patch.
Weather matters too. Cold, dry air dries out skin and triggers flares in 68% of people. Humid, warm weather helps 72% of patients feel better. If you live in a dry climate, use a humidifier in your bedroom. If you’re sun-sensitive, avoid direct sunlight during peak hours-though moderate sun can help some, it can hurt others.
The Bigger Picture: Science Is Catching Up
Researchers are now looking at the gut-skin connection. Early data suggests that probiotics may reduce flare frequency by 22% in people with imbalanced gut bacteria. High-fat diets, especially those rich in saturated fats, are also being studied-they can trigger inflammation through immune cells in the skin.
And the future? Wearable devices that track stress levels and AI apps that predict flares based on your habits are already in testing. Within five years, personalized trigger maps could become standard care, cutting flare frequency by 40-60%.
Right now, the most powerful tools you have are simple: protect your skin, manage stress, and treat infections fast. You can’t change your genes, but you can change how you respond to the world around you.
Can stress cause psoriasis, or just make it worse?
Stress doesn’t cause psoriasis on its own-you need the right genes. But it can trigger your first flare or make existing psoriasis much worse. Many people report their first outbreak happening within a year of a major stressful event. Stress activates immune pathways that inflame the skin, and it also weakens the skin barrier, making flares more likely.
Are infections the only trigger for guttate psoriasis?
Streptococcal infections-like strep throat, tonsillitis, or sinusitis-are the most common trigger for guttate psoriasis, especially in children and teens. But other infections, including viral ones like the flu or COVID-19, can also cause it. The key is that your immune system reacts to the infection by mistakenly targeting skin cells. Treating the infection early can help prevent the flare from spreading.
Why does my skin get worse in winter?
Cold, dry air strips moisture from your skin, and indoor heating makes it worse. This dries out your skin barrier, making it easier for inflammation to start. Sixty-eight percent of people with psoriasis say winter triggers their flares. Using a humidifier, moisturizing right after showers, and avoiding long hot showers can help. Some people also benefit from brief, controlled sun exposure-but always protect against burns.
Should I avoid certain foods to prevent flares?
Some people report that dairy, gluten, or nightshades (like tomatoes and peppers) make their psoriasis worse, but this isn’t true for everyone. A 2022 survey found 32% of patients linked dairy to flares, 25% to gluten. If you suspect a food trigger, try eliminating it for 4-6 weeks and track changes. Don’t cut out entire food groups without checking with a doctor-nutrition matters for overall immune health.
Can I use regular lotion for psoriasis?
Most regular lotions contain fragrances, alcohol, or harsh chemicals that can irritate psoriasis-prone skin. Instead, use thick, fragrance-free creams or ointments labeled for sensitive skin or eczema. Look for ingredients like ceramides, hyaluronic acid, or colloidal oatmeal. These help rebuild your skin’s natural barrier. Ointments (like petroleum jelly) work better than lotions because they lock in moisture longer.






Ashley Farmer
December 8, 2025 AT 01:11Just wanted to say this post saved my skin this winter. I started moisturizing right after showers like it said and used a humidifier. No more cracking, no more burning. It’s not magic, but it’s real.
Thank you for the science-backed hope.
Helen Maples
December 8, 2025 AT 23:15Stress doesn’t cause psoriasis, but it absolutely weaponizes it. I lost my job last year, went from 5% body coverage to 40% in six weeks. No one talks about how the shame of visible plaques compounds the stress. It’s a spiral, not a cycle. And yes, meditation helps-but only if you’re not too exhausted to sit still.
Sangram Lavte
December 9, 2025 AT 23:44Flu shot = psoriasis shield. Got mine last October. Zero flares since. My derm said it’s not proven, but I’m not risking another strep-triggered outbreak. Simple. Free. Do it.
Olivia Hand
December 10, 2025 AT 05:04I’ve been tracking my triggers for 11 months. 82% of flares followed either sleep deprivation or a fight with my partner. Not stress in general-specific emotional ruptures. That’s the real trigger. Not ‘bad week’-it’s ‘I felt abandoned.’ The body knows.
Desmond Khoo
December 11, 2025 AT 15:04Y’all are gonna laugh but I started using petroleum jelly on my elbows before bed. Like, straight from the jar. No fancy creams. No scent. Just Vaseline. Three weeks later, my plaques faded like they were never there. Sometimes the dumbest solution is the one that works.
🫶
Kyle Oksten
December 12, 2025 AT 12:01There’s a deeper truth here: psoriasis isn’t a skin disease. It’s a mirror. It reflects the chaos inside. When your life is fragmented, your skin fragments. Healing requires integration-not just ceramides, but meaning. You can’t moisturize your soul with lotion.
Wesley Phillips
December 12, 2025 AT 15:01Look I get it, but let’s be real-this post is basically a pharmaceutical ad disguised as science. Who paid for that JAMA study? Who funds the ceramide hype? The real cure is fasting and cold exposure. The system doesn’t want you to know that.
Stacy here
December 13, 2025 AT 15:48They told us stress causes flares. But what if it’s not stress? What if it’s the 5G towers? The glyphosate in our water? The government’s secret bioweapon targeting autoimmune patients? I’ve seen 17 people in my support group go from mild to severe after the new cell tower went up downtown. Coincidence? I think not.
Ernie Blevins
December 13, 2025 AT 19:52Everyone’s talking about moisturizers and meditation. What about the truth? Most of you are just lazy. You don’t want to change your diet. You don’t want to quit drinking. You don’t want to face your trauma. So you buy a $40 cream and call it a day. Wake up.
Sadie Nastor
December 14, 2025 AT 11:20I’m not gonna lie-I cried reading this. I thought I was broken. Turns out my skin was just screaming for help. I started journaling at night. Not even deep stuff. Just ‘today I felt okay’ or ‘today I felt alone.’ It’s not a cure, but it’s a lifeline. 🌱
Nancy Carlsen
December 14, 2025 AT 15:29As a Nigerian-American, I’ve seen how culture affects psoriasis care. In my family, hot water = clean. But that’s the worst thing for skin. I had to teach my mom that ‘clean’ doesn’t mean scalding. Now she uses oatmeal baths. We laugh about it. Healing isn’t just physical-it’s relational.
Ted Rosenwasser
December 16, 2025 AT 04:19Let’s cut through the noise. Ceramides are overrated. The real key is reducing IL-23 via biologics. If you’re not on a TNF-alpha inhibitor or an IL-17 blocker, you’re just doing yoga with your lotion. Don’t romanticize the struggle. Science has the answer. Go get prescribed.
Jennifer Anderson
December 17, 2025 AT 15:50my skin got better when i stopped washing my hair every day. i know that sounds wild but the sulfate shampoo was wrecking my scalp. now i use just water and apple cider vinegar rinse. no more flakes on my shoulders. who knew??
Nicholas Heer
December 17, 2025 AT 18:53They say stress triggers flares. But who’s stressing us out? The corporations that sell you expensive creams. The doctors who push meds. The media that makes you feel guilty for not meditating 20 minutes a day. This whole psoriasis narrative is a capitalist trap. Your skin is fine. The system is broken.
Ryan Sullivan
December 18, 2025 AT 00:29While the anecdotal evidence presented here is emotionally compelling, it lacks methodological rigor. Correlation does not imply causation. Without controlled longitudinal studies accounting for confounders like diet, microbiome diversity, and environmental toxins, these recommendations border on pseudoscientific. The burden of proof remains unmet.