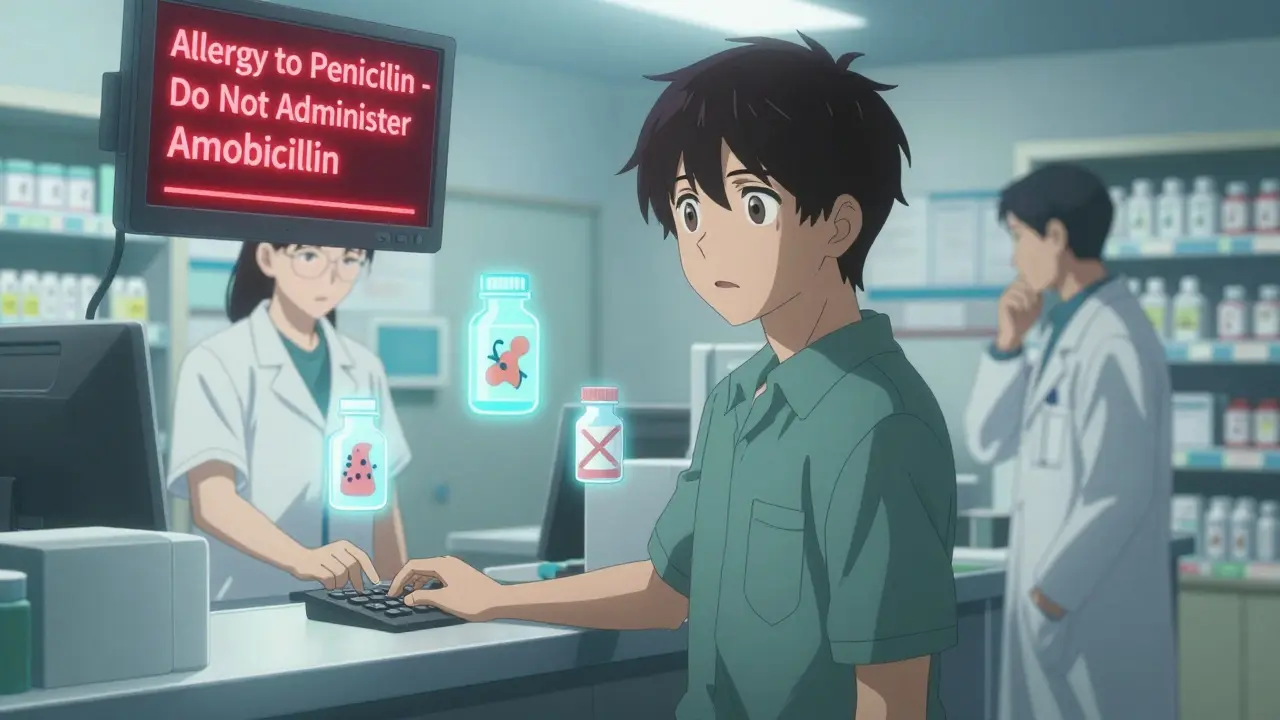
When you pick up a prescription, you might see a warning on the screen at the pharmacy: "Allergy to Penicillin - Do Not Administer Amoxicillin". It feels urgent. It feels like a lifesaver. But here’s the truth: more than half of these alerts are wrong. Or at least, they’re not as dangerous as they look.
What Are Pharmacy Allergy Alerts, Really?
Pharmacy allergy alerts are automated warnings built into hospital and pharmacy computer systems. They pop up when a doctor or pharmacist tries to prescribe or fill a medication that might conflict with a patient’s recorded allergy. These systems have been around since the late 1990s and now exist in nearly every U.S. hospital and pharmacy. Their goal is simple: prevent dangerous reactions. But the way they work? Not so simple. These alerts aren’t magic. They’re based on databases that link drugs to ingredients and cross-reactivity patterns. For example, if you’re listed as allergic to penicillin, the system might flag every drug in the penicillin family - amoxicillin, ampicillin - and even some unrelated drugs like cephalosporins, even though the real risk is often less than 2%. The system doesn’t know if your reaction was a rash, nausea, or anaphylaxis. It just sees the word "allergy" and sounds the alarm.The Two Types of Alerts You’ll See
Not all alerts are created equal. There are two main kinds:- Definite allergy alerts: These trigger when the medication matches an exact or class-based allergy in your record. For example, you’re documented as allergic to penicillin, and the system sees amoxicillin - a penicillin derivative. This one’s usually accurate.
- Possible allergy alerts: These are the troublemakers. They warn about cross-reactivity - like suggesting you might react to a cephalosporin because you’re "allergic" to penicillin. But here’s the kicker: over 90% of all alerts are this type. And most of them are unnecessary.
A 2020 study found that 90% of allergy alerts come from cross-reactivity assumptions, not real matches. And the truth? Modern cephalosporins (especially 3rd and 4th generation) have almost no cross-reactivity with penicillins. Yet systems still treat them like dangerous twins.
Why So Many Alerts Are Wrong - And Dangerous
The biggest problem? Poor documentation. Most patients don’t know the difference between a true allergy and a side effect. They say, "I had a stomachache after taking penicillin as a kid," and that gets recorded as "penicillin allergy." But stomachaches aren’t allergies. They’re side effects. Same with nausea from metformin, dizziness from beta-blockers, or headaches from aspirin. None of these are immune system reactions. Yet the system doesn’t care. It sees "allergy" and triggers a red flag. A 2019 study found that only 12% of NSAID allergy alerts actually represented real allergic reactions. The rest? Just confusion. And here’s the scary part: doctors and pharmacists override these alerts more than 95% of the time. Why? Because they’ve learned - the hard way - that most are noise. But when you override 95% of alerts, you start ignoring the 5% that could save your life. That’s alert fatigue, and it’s killing people.
What the Colors and Symbols Really Mean
Different systems use different ways to show severity. Epic Health uses color codes: yellow for mild, orange for moderate, red for severe, and black for life-threatening. Cerner uses icons and text labels. But here’s what you need to know: the color doesn’t always match the real risk. If your record says "penicillin allergy" with no details, the system might show a red alert for amoxicillin - even if your reaction was a harmless rash 20 years ago. That’s not risk stratification. That’s overkill. The best systems now try to fix this. Epic’s 2023 update introduced "Allergy Relevance Scoring" - a machine learning tool that looks at your history. If you’ve taken penicillin before without issue, or if your allergy was documented as "nausea," the alert gets downgraded. It’s a start.How to Read an Alert Like a Pro
When an alert pops up, don’t just click "OK." Ask yourself these four questions:- What was the actual reaction? Was it a rash? Hives? Swelling? Trouble breathing? Or just nausea, diarrhea, or headache? Only the first four are true allergies.
- When did it happen? True allergic reactions happen within minutes to hours after taking the drug. If it was weeks later, it’s likely not immune-related.
- Was it confirmed by a specialist? Most people are mislabeled. Only 1 in 10 people who think they’re allergic to penicillin actually are. A simple skin test can clear it up.
- Is this a class-based alert? If it’s warning you about a drug you’ve taken before - or one that’s not even in the same family - it’s probably wrong.
At Mayo Clinic, they started requiring pharmacists to document the exact reaction - not just "allergy." Within six months, accurate allergy records jumped from 39% to 76%. Fewer alerts. Fewer overrides. Safer care.
What You Can Do Right Now
You don’t have to wait for the system to fix itself. Here’s how to take control:- Clarify your own allergy history. If you’ve been told you’re allergic to penicillin, ask your doctor if you’ve ever been tested. Most people haven’t. A simple skin test or oral challenge can prove you’re not allergic - and open up safer, cheaper antibiotic options.
- Update your records. Don’t just say "allergic to penicillin." Say: "Had a rash after penicillin at age 7. No swelling, no breathing issues. Never tested." That changes the alert.
- Ask before you take it. If you’re told you can’t take a drug because of an allergy, ask: "Is this based on a real reaction? Or just a guess?"
- Bring your list to every appointment. Keep a written list of reactions - not just drug names. Include symptoms and timing. Give it to every provider.
The Future Is Smarter Alerts
Change is coming. The 21st Century Cures Act, which took effect in January 2023, now requires EHR systems to use structured allergy documentation - meaning you can’t just type "allergy" anymore. You have to pick from a dropdown: rash, hives, anaphylaxis, nausea, etc. Health systems like Kaiser Permanente and Intermountain Healthcare are already using AI to predict which alerts are truly dangerous. Oracle Health’s new "Precision Allergy" module pulls data from allergist visits. If you’ve had a drug challenge and were cleared, the system automatically lowers the alert level. By 2026, 70% of major systems will use risk-stratified alerts - meaning only true high-risk reactions trigger loud, mandatory warnings. Mild reactions? They’ll show up as quiet notes. That’s the future. And it’s already starting.Bottom Line: Don’t Trust the Alert - Trust the Details
Pharmacy allergy alerts aren’t evil. They’re well-intentioned. But they’re broken. They scream "danger!" when the risk is tiny. They punish patients for outdated, vague records. And they make providers numb to real emergencies. The fix isn’t better technology. It’s better information. You are the key. Know your history. Speak up. Correct your records. Ask questions. Because when it comes to your safety, no computer should make the final call.Are all drug allergy alerts accurate?
No. Over 90% of allergy alerts are triggered by cross-reactivity assumptions or vague documentation, not true immune reactions. Studies show that more than half of all alerts are for medications patients have safely taken before. Many alerts are for side effects like nausea or headache, which are not allergies.
What’s the difference between an allergy and a side effect?
An allergy involves your immune system reacting to a drug - symptoms include hives, swelling, trouble breathing, or anaphylaxis. Side effects are non-immune reactions like nausea, dizziness, or headaches. Only 5-10% of drug reactions are true allergies. The rest are side effects, which shouldn’t trigger the same level of alert.
Can I outgrow a drug allergy?
Yes. Many people, especially those who had a rash as a child, are no longer allergic. Studies show that 80% of people labeled with penicillin allergy lose their sensitivity within 10 years. The only way to know for sure is through testing - skin tests or supervised oral challenges - done by an allergist.
Why do pharmacists keep overriding allergy alerts?
Because most alerts are false or low-risk. Clinicians override alerts 95% of the time for non-severe reactions because they’ve learned the system over-predicts danger. This creates "alert fatigue," where even real threats get ignored. It’s a systemic problem, not just individual negligence.
Should I be worried if my allergy record says "penicillin allergy" but I’ve taken it before?
Yes - but not because you’re in immediate danger. It means your record is outdated or inaccurate. You should talk to your doctor about getting tested. If you’ve taken penicillin or amoxicillin since the allergy was recorded, you likely aren’t allergic. Correcting this can give you access to better, cheaper, and more effective antibiotics.
How can I help improve my allergy record?
Keep a written list of every drug you’ve taken and exactly what happened. Include symptoms, timing, and whether you saw a doctor. Bring this to every appointment. Ask your provider to update your EHR with precise language - not just "allergy," but "rash after penicillin at age 8, no breathing issues." This reduces false alerts and keeps you safer.


Juan Reibelo
January 23, 2026 AT 18:19I’ve seen this a hundred times-my grandma got flagged for "penicillin allergy" because she threw up once at 12. Turns out? She’s taken it five times since. No rash. No swelling. Just a bad stomach. But the system? Red alert. Every. Single. Time.
Pharmacists just click through it like it’s a pop-up ad. We’re all numb. And that’s the real danger.
Karen Conlin
January 23, 2026 AT 23:20THIS. This is why I keep a laminated card in my wallet. Not just drug names-exact symptoms, dates, whether I saw a doctor. I once had a nurse tell me I was "allergic to ibuprofen" because I got a headache once. Headache. Not hives. Not anaphylaxis. Just a headache. I corrected it on the spot. Now they call me "The Record Keeper."
Stop letting computers decide your treatment. You know your body better than an algorithm. Document. Clarify. Advocate. It’s not extra work-it’s survival.
asa MNG
January 24, 2026 AT 09:24Sawyer Vitela
January 24, 2026 AT 14:27Amelia Williams
January 25, 2026 AT 21:09I’m a nurse, and I’ve watched this play out for 12 years. The worst part? Kids get labeled with "allergy" because their mom says they got a tummy ache after antibiotics. Then they grow up on clindamycin or vancomycin-way more expensive, way more toxic-just because no one bothered to ask, "What exactly happened?"
It’s not just about saving money. It’s about saving their kidneys. Their guts. Their future. We need to stop treating documentation like a checkbox.
Viola Li
January 26, 2026 AT 15:00venkatesh karumanchi
January 27, 2026 AT 06:26In India, we don’t have fancy EHR systems. But we do have doctors who ask questions. My uncle was told he was allergic to penicillin. He never was. He just had a fever when he took it. The doctor said, "Fever doesn’t mean allergy." Simple. Human. Effective.
Technology is great-but it can’t replace a good conversation.
Jenna Allison
January 28, 2026 AT 10:07As a pharmacist, I see this daily. The system flags cephalosporins for penicillin allergies-even though the cross-reactivity risk is less than 1% for 3rd-gen. But if I override it without documenting why, I get audited. So I do. But I also call the patient’s PCP and say, "Hey, this record says "allergy," but the patient says they took it last year fine. Can we update?"
It’s not the tech’s fault. It’s the workflow. We need structured fields, not free text. And we need to reward documentation, not punish overrides.
Kat Peterson
January 30, 2026 AT 02:03Izzy Hadala
January 31, 2026 AT 12:27It is imperative to acknowledge that the current paradigm of automated allergy alerting, as implemented in most electronic health record systems, is predicated upon binary, categorical, and non-contextual data inputs. This methodology inherently lacks the nuance required to differentiate between immunoglobulin E-mediated reactions and non-immunologic adverse drug events. Consequently, the resulting alerting architecture exhibits a high false-positive rate, which, in turn, engenders clinical desensitization-a phenomenon well-documented in the human factors literature as "alert fatigue." The solution, therefore, necessitates not merely technological enhancement, but a paradigmatic shift toward granular, structured, and longitudinal patient-reported outcome integration.
Tommy Sandri
February 2, 2026 AT 08:13As a physician who has practiced across three countries, I’ve seen how this issue varies culturally. In the U.S., patients are quick to self-diagnose allergies. In Germany, they’re more likely to say, "I had a reaction once, but I didn’t see a doctor." In Japan, they often avoid mentioning it altogether. The system doesn’t adapt to that. It just screams.
We need global standards for allergy documentation-not just in EHRs, but in how patients are educated. This isn’t a tech problem. It’s a communication problem.