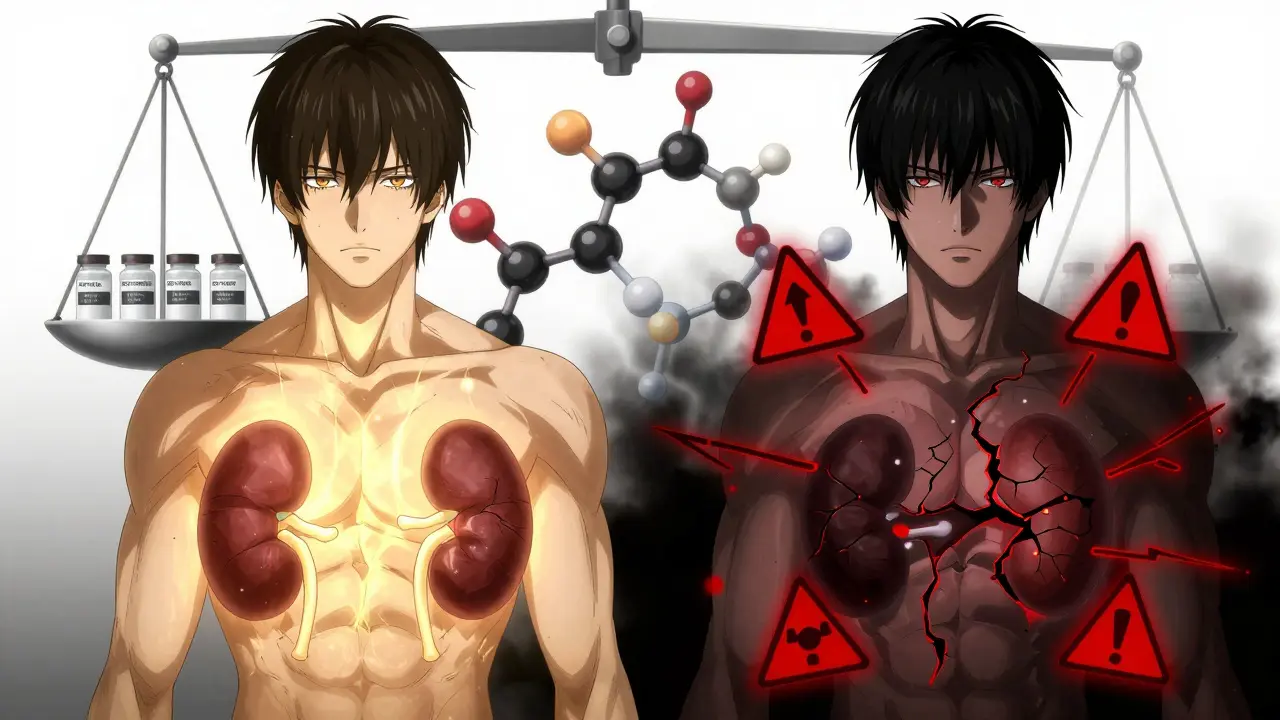
When someone takes cyclosporine after a kidney, liver, or heart transplant, their life depends on getting the dose just right. Too little, and the body rejects the new organ. Too much, and the kidneys fail, the liver gets damaged, or seizures kick in. The margin between life-saving and life-threatening is razor-thin. But here’s the catch: cyclosporine doesn’t just sit there quietly. It actively messes with how your body processes dozens of other drugs - and those other drugs mess with it in return. This isn’t just a footnote in a prescribing guide. It’s a daily clinical challenge that can mean the difference between a successful transplant and an emergency room visit.
Why CYP3A4 Matters More Than You Think
CYP3A4 is the most common enzyme in your liver and gut. It’s like a molecular trash compactor for drugs. About 60% of all medications you take - from statins to antibiotics to painkillers - get broken down by this one enzyme. If CYP3A4 slows down, those drugs build up. If it speeds up, they vanish before they can work. Cyclosporine doesn’t just pass through this system. It jams it. It binds to CYP3A4, blocks its active site, and stops it from doing its job. This isn’t a temporary glitch. It’s a sustained, dose-dependent inhibition that lasts as long as cyclosporine is in your bloodstream.
What makes this even trickier is that cyclosporine itself is a substrate of CYP3A4. That means your body uses the same enzyme to clear cyclosporine out of your system. So if something else inhibits CYP3A4 - like grapefruit juice, clarithromycin, or diltiazem - cyclosporine levels can skyrocket. And if something induces CYP3A4 - like rifampin or St. John’s wort - cyclosporine gets cleared too fast. Both scenarios are dangerous. One leads to toxicity. The other leads to rejection.
How Cyclosporine Compares to Other Immunosuppressants
Many people assume all transplant drugs behave the same. They don’t. Tacrolimus, the other main calcineurin inhibitor, is mostly a substrate of CYP3A4 - meaning it gets metabolized by the enzyme, but doesn’t strongly inhibit it. Cyclosporine, on the other hand, is both a substrate and a potent inhibitor. This gives it a dual role: it can raise levels of other drugs and have its own levels altered by other drugs. That’s why you’ll see more interaction warnings with cyclosporine than with tacrolimus.
For example, when a transplant patient starts taking sirolimus (another immunosuppressant), the combination with cyclosporine can cause sirolimus blood levels to jump by over 200%. That’s why guidelines say you must reduce sirolimus by about 70% if it’s used with cyclosporine. But if the same patient were on tacrolimus, you wouldn’t see this kind of spike - because tacrolimus doesn’t inhibit sirolimus metabolism. This difference is why some transplant centers still use cyclosporine in specific cases: it’s predictable, but only if you know exactly what you’re dealing with.
The Hidden Role of P-Glycoprotein
CYP3A4 isn’t the only player. Cyclosporine also blocks P-glycoprotein (P-gp), a transporter protein that pumps drugs out of cells - especially in the gut, blood-brain barrier, and kidneys. This means cyclosporine doesn’t just slow drug breakdown. It also stops drugs from being cleared from tissues. So even if a drug is metabolized by a different enzyme, cyclosporine can still trap it in your system.
This dual action explains why some interactions are worse than expected. Take digoxin, a heart drug. It’s not primarily metabolized by CYP3A4 - it’s mainly cleared by P-gp. But when cyclosporine is added, digoxin levels can rise by 50-100%. That’s not just a lab curiosity. That’s a risk of fatal arrhythmias. No other common immunosuppressant does this. It’s a unique fingerprint of cyclosporine.
Real-World Consequences: What Happens When Things Go Wrong
Let’s say a patient gets a kidney transplant and is stable on cyclosporine. Their levels are steady at 180 ng/mL - perfect. Then they get a sinus infection. Their doctor prescribes clarithromycin, a strong CYP3A4 inhibitor. Within 48 hours, their cyclosporine level jumps to 650 ng/mL. They start vomiting, their creatinine spikes, and their blood pressure crashes. This isn’t rare. A 2021 study of over 1,200 transplant patients found that nearly one in three had at least one major drug interaction involving cyclosporine. Over 8% ended up hospitalized.
On the flip side, a patient on rifampin for tuberculosis - a strong CYP3A4 inducer - can see their cyclosporine levels drop by 70%. Within days, their body starts attacking the transplanted organ. Acute rejection. Another hospitalization. Another surgery. These aren’t hypotheticals. They’re documented in transplant journals worldwide.
Managing the Risk: What Clinicians Do
There’s no magic bullet. But there are clear steps that work:
- Map every drug - including OTC meds, supplements, and herbal products. Even something as simple as a calcium supplement can interfere with absorption.
- Check for CYP3A4 inhibitors and inducers - common ones include azole antifungals (ketoconazole), macrolide antibiotics (erythromycin), antivirals (ritonavir), and anticonvulsants (carbamazepine).
- Monitor levels before and after changes - cyclosporine trough levels should be checked within 24-72 hours of starting or stopping any interacting drug.
- Adjust doses proactively - if adding a moderate inhibitor like diltiazem, reduce cyclosporine by 25-50%. If adding a strong one like clarithromycin, cut it by 50-75% and prepare for daily monitoring.
- Use electronic alerts - hospitals with integrated EHR systems that flag potential interactions have seen a 45% drop in adverse events.
Some centers now use pharmacogenetic testing. About 15% of people have genetic variants in CYP3A4 that make them slow metabolizers. These patients need lower starting doses. Others are ultra-rapid metabolizers - they need more. This isn’t sci-fi. It’s standard practice in leading transplant centers in Europe and the U.S.

What Patients Need to Know
If you’re on cyclosporine, you’re not just managing one drug. You’re managing a web of interactions. You need to:
- Never start a new medication - even an OTC one - without checking with your transplant team.
- Avoid grapefruit, Seville oranges, and pomelos. They’re not just bad for statins - they’re dangerous with cyclosporine.
- Report any new symptoms: nausea, tremors, swollen gums, high blood pressure, or changes in urination.
- Keep a written list of all your drugs and bring it to every appointment.
- Know your target cyclosporine level. Ask your doctor what it is and why.
There’s no room for guesswork. A single change in one drug can undo months of careful management.
The Future: Personalized Dosing and Real-Time Monitoring
Research is moving fast. A 2023 study from Wenzhou Medical University showed that combining CYP3A4 genotype data with current medications lets doctors predict cyclosporine levels with over 85% accuracy. That’s huge. It means future dosing won’t be based on weight or age - it’ll be based on your biology.
Point-of-care devices are also in the works. Imagine a handheld monitor that gives you your cyclosporine level in 10 minutes, right in your doctor’s office. Prototypes are already showing 95% correlation with lab tests. This could make daily monitoring routine, not rare.
For now, the rules are simple: know your drugs, know your levels, and never assume. Cyclosporine is still a cornerstone of transplant medicine - not because it’s perfect, but because when managed right, it saves lives. And that only happens when the interactions are understood, tracked, and controlled.
Can grapefruit juice really affect cyclosporine levels?
Yes. Grapefruit juice is one of the most potent natural inhibitors of CYP3A4. Even a single glass can increase cyclosporine blood levels by 50-200%, depending on the person. This effect lasts for days. There’s no safe amount. Patients on cyclosporine are strongly advised to avoid all forms of grapefruit, Seville oranges, and pomelos - including juices, jams, and supplements.
Is cyclosporine still used today, or has it been replaced?
Tacrolimus is now the first-choice immunosuppressant for most adult transplant patients because it’s more effective and has fewer side effects like gum overgrowth or tremors. But cyclosporine is still widely used - especially in children, patients with certain autoimmune diseases like nephrotic syndrome, and in regions where cost is a barrier. It remains on the WHO’s List of Essential Medicines. Its use hasn’t disappeared; it’s just more targeted.
How often should cyclosporine levels be checked?
When starting cyclosporine, levels are checked daily for the first week, then weekly for the first month. Once stable, checks may drop to every 2-4 weeks. But anytime a new drug is added or removed - even a simple antibiotic - levels must be rechecked within 2-3 days. This isn’t optional. It’s standard of care.
Can I take over-the-counter pain relievers with cyclosporine?
Acetaminophen (Tylenol) is generally safe at normal doses. NSAIDs like ibuprofen or naproxen are riskier - they can worsen kidney function and may interact with cyclosporine’s effect on blood flow to the kidneys. Always check with your transplant team before taking any OTC painkiller. Even a few days of NSAID use can push someone into kidney failure.
What happens if I miss a dose of cyclosporine?
Missing one dose occasionally won’t cause rejection, but it can cause fluctuations in blood levels that make monitoring harder. If you miss a dose, take it as soon as you remember - unless it’s close to the next scheduled dose. Then skip it. Never double up. Consistency matters more than perfection. But if you miss multiple doses, contact your transplant team immediately. Your level could drop below the therapeutic range.
Managing cyclosporine isn’t about memorizing a list of drugs. It’s about understanding a system - how your body processes medication, how other drugs interfere, and how your own biology plays a role. The goal isn’t to avoid cyclosporine. It’s to use it safely. And that takes awareness, vigilance, and communication - not just with your doctor, but with every provider, pharmacist, and even family member who helps manage your care.





steve sunio
February 14, 2026 AT 21:43athmaja biju
February 15, 2026 AT 08:44Robert Petersen
February 16, 2026 AT 20:41Craig Staszak
February 17, 2026 AT 20:21Alyssa Williams
February 18, 2026 AT 22:06Ernie Simsek
February 19, 2026 AT 03:40Carla McKinney
February 19, 2026 AT 09:45Kristin Jarecki
February 21, 2026 AT 00:35Rachidi Toupé GAGNON
February 22, 2026 AT 08:57Jim Johnson
February 24, 2026 AT 00:01