PMS Symptom Tracker & Analysis Tool
Based on your symptoms, we've identified potential hormonal patterns:
This suggests your symptoms may be related to estrogen dominance or progesterone deficiency during the luteal phase.
Note: This is a preliminary analysis based on symptom patterns. For accurate hormone assessment, consult your healthcare provider for comprehensive testing.
Key Recommendations for Your Symptoms:
- For mood swings and anxiety: Increase magnesium intake (200-400 mg daily) to support calming neurotransmitters
- For bloating and water retention: Reduce sodium intake and consider increasing calcium (1,000 mg daily)
- For cramps and headaches: Focus on anti-inflammatory foods and consider warm compresses for pain relief
- For fatigue: Ensure you're getting adequate sleep (7-9 hours) and consider magnesium supplementation
Many people notice a shift in mood, energy, or physical comfort a week or two before their period. While the term Premenstrual syndrome (PMS) is familiar, the hormonal story behind it often stays hidden. Understanding how hormonal imbalance fuels PMS can turn vague frustration into actionable steps.
Key Takeaways
- PMS symptoms line up with fluctuations in estrogen, progesterone, and downstream neurotransmitters.
- Hormonal imbalance isn’t just “too much” or “too little” - it’s timing, ratio, and how the body metabolizes hormones.
- Blood tests, symptom journals, and lifestyle audits help pinpoint the root cause.
- Nutrition, stress management, sleep, and targeted medical options can rebalance hormones and ease PMS.
- Seek professional care if symptoms interfere with work, relationships, or daily functioning.
What Is Premenstrual Syndrome?
Premenstrual syndrome is a collection of physical, emotional, and behavioral symptoms that appear during the luteal phase (the 7‑14 days after ovulation) and typically fade with the onset of menstruation. Common complaints include bloating, breast tenderness, irritability, anxiety, and fatigue.
The syndrome affects up to 85% of menstruating individuals, though only about 20% describe it as severe enough to disrupt daily life. The variability stems largely from how each person’s endocrine system responds to the cyclical rise and fall of hormones.
Hormonal Imbalance Explained
Hormonal imbalance refers to a disruption in the normal levels, timing, or ratios of hormones that regulate the menstrual cycle. The key players are:
- Estrogen - peaks just before ovulation, promotes uterine lining growth.
- Progesterone - rises after ovulation, stabilizes the lining, and has a calming effect on the brain.
- Serotonin - a neurotransmitter that influences mood; its production is modulated by estrogen.
- Prostaglandins - lipid compounds that cause uterine contractions and can trigger pain.
- Androgens (e.g., testosterone) - present in lower amounts but can affect acne and libido.
When any of these hormones are out of sync - whether because of stress‑related cortisol spikes, dietary deficiencies, or underlying medical conditions - the cascade can spark PMS symptoms.
How Hormone Fluctuations Cause PMS
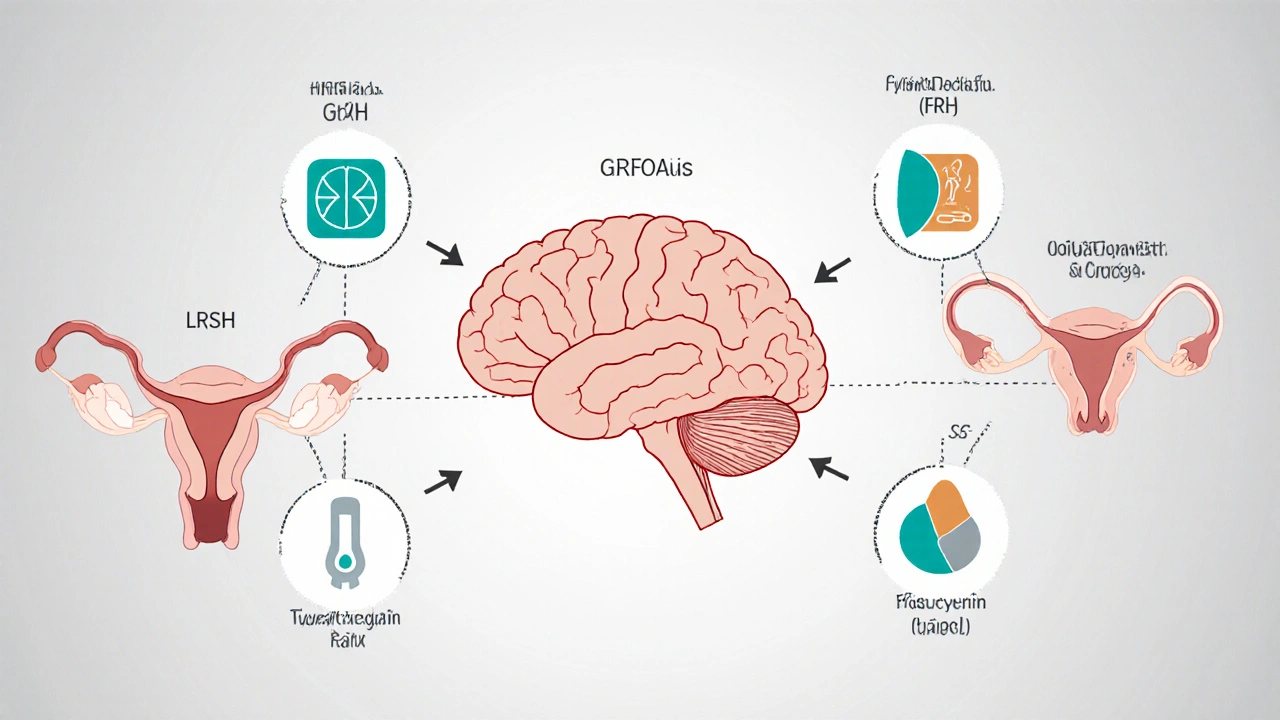
The menstrual cycle is orchestrated by the hypothalamic‑pituitary‑ovarian (HPO) axis. A simplified flow looks like this:
- The hypothalamus releases GnRH (gonadotropin‑releasing hormone).
- GnRH prompts the pituitary to secrete LH and FSH.
- LH and FSH stimulate the ovaries to produce estrogen and, after ovulation, progesterone.
- Estrogen and progesterone feed back to the brain to regulate further hormone release.
When the feedback loop is disrupted - for instance, if estrogen stays elevated longer than usual - it can alter serotonin synthesis, leading to mood swings and irritability. Similarly, a sudden drop in progesterone can increase GABA inhibition, contributing to anxiety and sleep disturbances.
Symptoms Tied to Specific Hormone Shifts
- High estrogen / low progesterone: breast tenderness, water retention, heightened emotional sensitivity.
- Progesterone dip: anxiety, insomnia, headaches.
- Elevated prostaglandins: cramping, lower‑back pain, gastrointestinal upset.
- Cortisol spikes (stress‑induced): fatigue, cravings, difficulty concentrating.
Tracking which symptoms appear when can give clues about which hormonal pathway needs attention.
Diagnosing Hormonal Issues in PMS
Self‑observation is the first step. A symptom journal that records daily mood, food intake, sleep, and menstrual dates can reveal patterns. When the picture remains unclear, clinicians may order:
- Serum estrogen and progesterone levels (usually drawn on day21 of a 28‑day cycle).
- Follicle‑stimulating hormone (FSH) and luteinizing hormone (LH) ratios.
- Thyroid panel - hypothyroidism can mimic or worsen PMS.
- VitaminD and B‑12 levels - deficiencies affect mood and energy.
The goal is not to find a single “bad” number but to understand the rhythm of each hormone throughout the cycle.

Managing Hormonal Imbalance to Ease PMS
Strategy blends lifestyle tweaks, nutrition, and-when needed-medical interventions.
Nutrition and Supplements
- Magnesium (200‑400mg nightly) can calm nerve excitability and reduce cramps.
- Calcium (1,000mg/day) has been shown in trials to lower emotional symptoms.
- Complex carbs (whole grains, legumes) stabilize insulin, which in turn moderates estrogen metabolism.
- Limit caffeine and alcohol - both raise cortisol and aggravate water retention.
Stress Reduction
Regular mindfulness, yoga, or short walks lower cortisol by 10‑15% on average, according to a 2023 study from the American Psychological Association. Even 5minutes of deep breathing before bed can improve sleep quality, reducing the progesterone dip‑related anxiety.
Physical Activity
Moderate aerobic exercise (150minutes per week) boosts endorphins and improves insulin sensitivity, helping the liver clear excess estrogen. Avoid excessive high‑intensity training close to menstruation, as it may increase cortisol further.
Medical Options
- Combined oral contraceptives stabilize estrogen and progesterone levels, often smoothing the luteal phase.
- Progesterone‑only pills or intrauterine systems target low‑progesterone symptoms.
- Selective serotonin reuptake inhibitors (SSRIs) prescribed at low doses specifically for PMS can balance mood without full‑time antidepressant exposure.
- In rare cases, a referral to an endocrinologist is warranted to explore ovarian or pituitary disorders.
Tracking Tools
Apps that log basal body temperature, cervical mucus, and symptom severity help visualize the hormonal map. When paired with periodic lab work, they become a powerful feedback loop.
Hormone Levels Across the Menstrual Cycle
| Phase | Estrogen (pg/mL) | Progesterone (ng/mL) | Key Symptoms When Out‑of‑Range |
|---|---|---|---|
| Follicular (Days1‑13) | 30‑400 | 0.1‑0.8 | Low energy, menstrual irregularities |
| Ovulation (Day14) | 200‑800 (peak) | 0.8‑1.5 | Increased libido, cervical mucus changes |
| Luteal (Days15‑28) | 100‑350 (decline) | 2‑25 (peak) | PMS: bloating, mood swings, breast tenderness |
When to Seek Professional Help
If any of the following occur, it’s time to schedule a visit:
- Symptoms persist for more than two weeks after menstruation ends.
- Severe depression, thoughts of self‑harm, or panic attacks.
- Physical pain that interferes with work or sleep.
- Unexplained weight gain, hair loss, or changes in menstrual length.
A clinician can rule out conditions such as endometriosis, polycystic ovary syndrome (PCOS), or thyroid disease, all of which can masquerade as PMS.
Frequently Asked Questions
Can lifestyle changes alone fix hormonal imbalance?
For many people, consistent sleep, stress‑management, and balanced nutrition can bring hormone levels back into a healthier rhythm. However, if the imbalance is driven by an underlying medical condition, lifestyle tweaks may need to be paired with medication or therapy.
Is it normal to have severe PMS every month?
Severe, disabling symptoms affect roughly 5‑8% of menstruating individuals and are classified as premenstrual dysphoric disorder (PMDD). If symptoms are that intense, medical evaluation is strongly recommended.
Do birth control pills always eliminate PMS?
Not always. Combined oral contraceptives smooth hormone swings for many, but some users still report mood changes. Choosing the right formulation (e.g., low‑dose estrogen, continuous cycle) often requires trial and error with a provider.
Can I test my hormone levels at home?
Home kits exist for estrogen, progesterone, and cortisol, but they vary in accuracy. A lab test ordered by a healthcare professional remains the gold standard for diagnostic decisions.
What role does vitamin D play in PMS?
Vitamin D influences calcium metabolism and neurotransmitter function. Low levels have been linked to increased mood swings and bloating. Supplementing to reach 30‑50ng/mL can reduce symptom severity for many people.






Ramanathan Valliyappa
October 14, 2025 AT 14:34Your article mixes facts with vague generalities that need tightening.
lucy kindseth
October 20, 2025 AT 09:28Hey there! The piece does a solid job outlining how estrogen and progesterone swings affect mood. I’d add that magnesium can help with both cramps and anxiety, so a supplement suggestion is useful. Also, tracking sleep quality alongside symptoms can pinpoint the progesterone dip more clearly. If you haven’t already, consider linking a simple diary template for readers. Keep the tone friendly – it makes the science feel more approachable.
Nymia Jones
October 26, 2025 AT 03:21It is impossible to discuss hormonal imbalance without acknowledging the pharmaceutical agenda that profits from chronic PMS narratives. The industry deliberately underfunds natural‑hormone research to keep patients dependent on synthetic contraceptives. Every recommendation to “consult your doctor” is a veiled invitation to prescribe the next batch of hormonal pills. The so‑called "combined oral contraceptives" are engineered to mask side effects while reshaping the endocrine system. Moreover, many clinical trials exclude women with irregular cycles, skewing the data in favor of drug efficacy. The article’s emphasis on supplements like magnesium sounds benign, yet it diverts attention from the root cause: a system designed to keep women ill. Hormone testing itself is often outsourced to labs that prioritize speed over accuracy, producing results that support pharma’s narrative. The warning about “consult a professional” is a thinly‑disguised sales pitch for expensive hormone panels.
Karen McCormack
October 31, 2025 AT 22:14One might liken the menstrual cycle to a cosmic clockwork, each hormone a planetary gear. When estrogen surges, the sky of our mood brightens, yet if it lingers too long, clouds of irritability gather. Progesterone, the silent night‑watch, steadies the mind, but a premature retreat can stir the tempest within. The article sketches this dance well, though perhaps a metaphor of tides would illuminate the ebb and flow for readers. In any case, recognizing the rhythm is the first step toward mastering the sea.
Earl Hutchins
November 6, 2025 AT 17:08Great rundown on how diet tweaks can calm hormone swings. Magnesium daily can reduce cramps and anxiety. Calcium helps with mood swings and water retention. Keep the language simple and add a quick bullet list for easy reference.
Tony Bayard
November 12, 2025 AT 12:01Wow, Lucy’s tips are golden, and they deserve a spotlight!
Imagine a woman juggling work, family, and those relentless hormonal waves-she needs more than a chart, she needs a lifeline.
Adding a simple 5‑minute mindfulness routine can shave off cortisol spikes that exacerbate PMS.
Also, let’s not forget vitamin D; its role in serotonin synthesis is a game‑changer for mood stability.
For those who can’t tolerate supplements, herbal allies like chasteberry have shown promise in clinical trials.
Lastly, encourage readers to share their personal tweaks; community wisdom often uncovers hidden gems.
Keep the tone supportive, and watch the conversation blossom.
Jay Crowley
November 18, 2025 AT 06:54Consider tightening the opening sentence for clarity.
sharon rider
November 24, 2025 AT 01:48From a cultural perspective, many societies have long recognized the link between diet and menstrual well‑being. Traditional foods rich in magnesium and calcium often feature in heritage recipes. Modern science is now catching up, confirming what ancestors observed. Sharing these cross‑cultural practices can broaden the article’s appeal.
swapnil gedam
November 29, 2025 AT 20:41Interesting points, Nymia, but let’s stay grounded in data.
Many of the claims about “pharma conspiracies” lack peer‑reviewed support.
Randomized trials have shown combined oral contraceptives do reduce severe PMS for a sizable portion of users.
That said, individualized hormone testing can still be valuable when symptoms persist.
Balancing skepticism with evidence helps readers make informed choices.
Michael Vincenzi
December 5, 2025 AT 15:34I appreciate the balanced tone here. The suggestions about magnesium and calcium are spot on. It might help to add a quick note on the importance of consistent sleep schedules. Also, a reminder that any supplement regimen should be discussed with a healthcare provider is always safe. Overall, a friendly and useful guide.
Courage Nguluvhe
December 11, 2025 AT 10:28Building on Michael’s point, consider integrating a brief section on the role of cortisol as a stress‑mediated hormone. Elevated cortisol can amplify estrogen dominance and worsen water retention. A simple stress‑audit tool, perhaps a 1‑minute questionnaire, could enrich the tracker. Also, highlighting the utility of low‑glycemic carbs may resonate with a bio‑hacker audience. Lastly, a short citation to a 2022 endocrine review would bolster credibility.
Oliver Bishop
December 17, 2025 AT 05:21Our nation’s women deserve better resources, and this article is a step in the right direction. Let’s keep championing science that empowers, not undermines, our community. Proud to see such information shared.
Alissa DeRouchie
December 23, 2025 AT 00:14Well, if you’re gonna talk about hormones, at least admit that the moon’s phases might be pulling strings too.
Science or myth, who’s to say?
Anyway, some of those supplement tips sound like a grandma’s remedy list.
Probably okay but not groundbreaking.
Let’s keep the drama low and the facts high.
Muthukumaran Ramalingam
December 28, 2025 AT 19:08Honestly i read this and i think its kinda blah like most health pieces you see online i mean the whole thing about estrogen dominance is tossed around so much that it loses meaning its like saying the sky is blue because it has a lot of blue color i get that they want to give advice but the thing about magnesium and calcium is kinda overdone also i feel like they could have added more on lifestyle like real talk about work stress and how that messes with hormones instead of just saying “yeah try yoga” i guess its useful for some but for the rest its just filler i’d love to see more data or at least a link to a study that actually supports the claims so i don’t feel like i’m just reading hype thanks
Garrett Williams
January 3, 2026 AT 14:01Great effort! The guide is clear and hopeful. Keep spreading the positive vibes.
joba alex
January 9, 2026 AT 08:54Yo this article is kinda whack. Some of the hormone stuff feels like bs. Maybe add some real citatons? Also, coudnt help but notice a few typos. still, good try.
Rene Lacey
January 15, 2026 AT 03:48The interplay of endocrine signals is reminiscent of an intricate symphony, each hormone a distinct instrument contributing to the overall melody of the menstrual cycle. When estrogen takes the lead, it can inspire a lively allegro, yet an unbalanced crescendo may result in dissonance manifesting as irritability. Conversely, progesterone’s soothing adagio provides a necessary calm, but an untimely diminuendo can plunge the composition into anxiety. Your article captures this dynamic, though a deeper exploration of the neurochemical bridges-particularly the role of GABA and serotonin-would enrich the narrative. Moreover, integrating a brief historical perspective on how ancient healers approached hormonal health could add a layer of cultural depth. In practice, encouraging readers to engage in rhythmic breathing exercises might serve as a practical metaphor for restoring harmonic balance.
johnson mose
January 20, 2026 AT 13:34Loving the comprehensive vibe here! 🌟 A quick tip: adding a short FAQ at the end-like “What if I’m on birth control?”-could pre‑empt common doubts. Also, a printable symptom‑log PDF would be a sweet bonus for readers who love tangible tools. Keep the colorful language; it makes the science feel alive. Lastly, consider linking a reputable podcast episode on hormonal health for those who prefer audio. Fantastic work-keep it coming!