Antiarrhythmic Medication Selector
Select Patient Information
Recommended Medication:
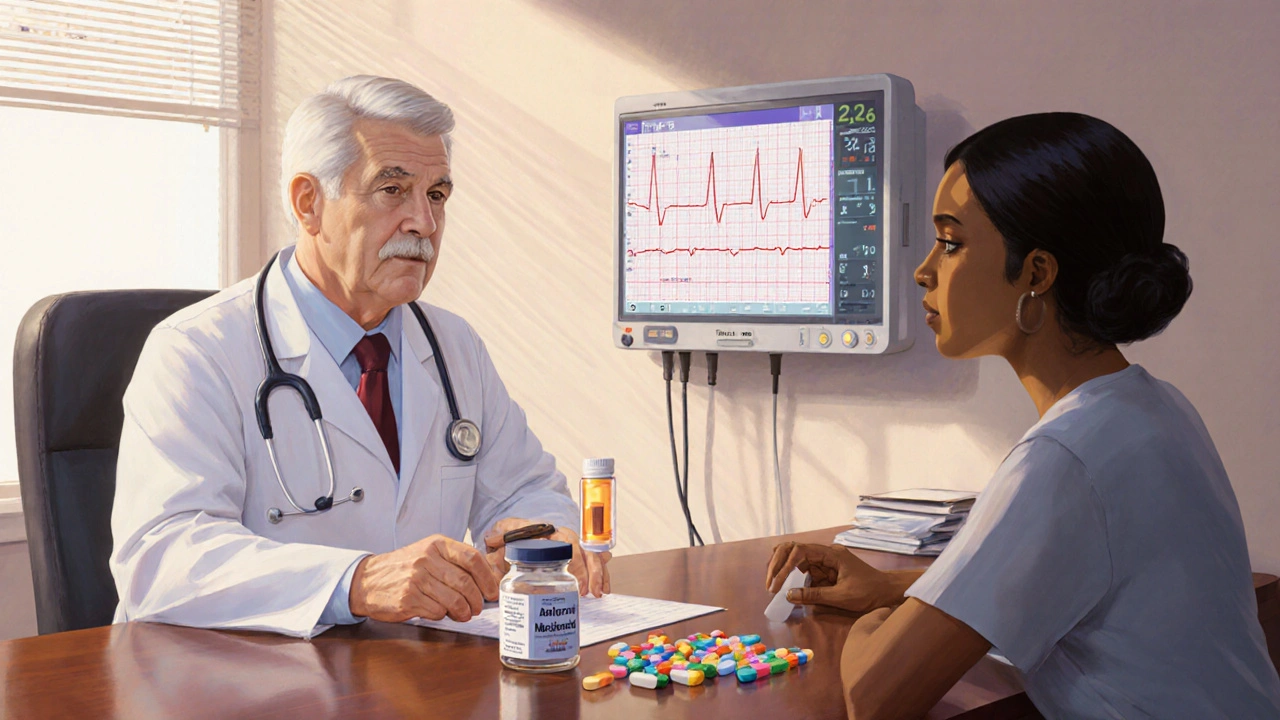
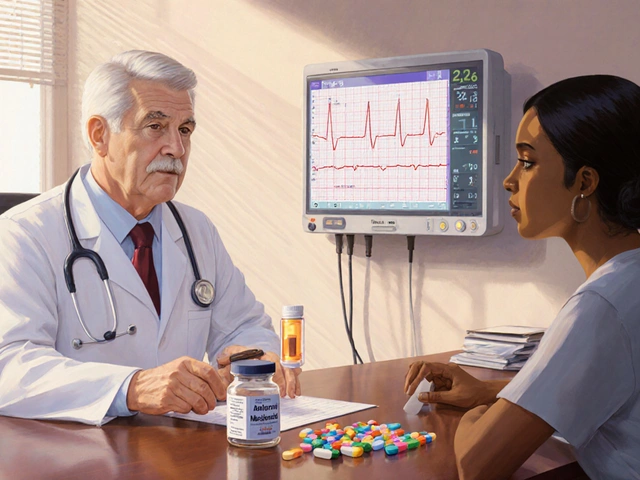
When a doctor prescribes a medication to keep an irregular heartbeat in check, the name on the bottle often sparks a cascade of questions: How does it work? What side effects should I watch for? Are there other drugs that might suit me better?
One of the most talked‑about drugs in this space is Amiodarone, also marketed as Cordarone. It's a powerhouse for treating life‑threatening arrhythmias, but its long‑term profile can feel like a double‑edged sword. Below, we break down how Amiodarone stacks up against the most common alternatives, so you can understand the trade‑offs before you or a loved one makes a decision.
Quick Summary
- Amiodarone is highly effective for ventricular and atrial fibrillation but carries a long half‑life and notable organ toxicities.
- ClassIII agents like Dofetilide and Sotalol are safer for short‑term use but need strict renal monitoring.
- ClassIC drugs (Flecainide, Propafenone) work well for atrial fibrillation in patients without structural heart disease.
- Beta‑blockers (Metoprolol) and calcium channel blockers (Verapamil) control rate rather than rhythm and have a milder side‑effect profile.
- Choosing the right drug hinges on the type of arrhythmia, underlying heart structure, comorbidities, and how closely you can follow lab tests.
Understanding Amiodarone (Cordarone)
Amiodarone is a classIII antiarrhythmic that prolongs the cardiac action potential by blocking potassium channels. It also has modest sodium, calcium, and beta‑blocking activity, which gives it a broad spectrum of effect. Because of this multitargeted action, Amiodarone can suppress both ventricular tachycardia and atrial fibrillation, making it a go‑to when other drugs fail.
Key attributes:
- Half‑life: 40‑60 days (some tissue stores linger for months).
- Typical dose: 200mg daily after a loading phase.
- Monitoring: Liver enzymes, thyroid function, pulmonary function, and ocular exams every 6months.
These long‑term monitoring requirements are the primary reason many patients and clinicians look for alternatives.
Top Alternatives and When They Shine
Below are the most frequently considered options, grouped by class and therapeutic niche.
ClassIII - Pure Potassium Channel Blockers
Dofetilide is a highly selective IKr blocker. It works well for converting atrial fibrillation to sinus rhythm and for maintenance therapy.
Pros: No long‑term tissue accumulation, quicker washout (half‑life ~10hours). Cons: Requires inpatient initiation and strict renal dosing.
Sotalol combines classIII activity with non‑selective beta‑blocking. It's often chosen for patients who need both rate and rhythm control.
Pros: Oral dosing, lower cost. Cons: Risk of torsades de pointes if QT prolongs; must monitor electrolytes and renal function.
ClassIC - Sodium Channel Blockers
Flecainide is effective for atrial fibrillation and some supraventricular tachycardias when the heart is structurally normal.
Pros: Rapid onset, good for “pill‑in‑the‑pocket” conversion. Cons: Can be pro‑arrhythmic in patients with coronary disease or left‑ventricular dysfunction.
Propafenone shares many traits with Flecainide but also has mild beta‑blocking activity, which can help with rate control.
Pros: Similar efficacy, modest effect on heart rate. Cons: Same structural‑heart contraindications; may cause taste disturbances.
Rate‑Control Options (Not Rhythm Converters)
For many patients, simply slowing the heart rate is enough. The two most common agents are:
Metoprolol, a cardioselective beta‑blocker, reduces sympathetic drive and is especially useful after myocardial infarction.
Verapamil, a non‑dihydropyridine calcium‑channel blocker, slows AV‑node conduction and can be combined with anticoagulation for atrial fibrillation.
These drugs don’t restore normal rhythm but are easier to monitor and have fewer severe organ toxicities compared with Amiodarone.
Legacy Agents with Niche Roles
Digoxin is a cardiac glycoside that increases vagal tone, lowering ventricular rate in atrial fibrillation. It’s rarely used as a first line today because of its narrow therapeutic window, but it can be useful in sedentary patients with heart failure who can’t tolerate beta‑blockers.
Side‑Effect Profiles at a Glance
Understanding side‑effects helps you weigh the benefits against the risks. Below is a concise side‑effect matrix for the drugs discussed.
| Drug | Class | Key Indications | Half‑Life | Common Side‑Effects | Major Contra‑indications | Monitoring Needs |
|---|---|---|---|---|---|---|
| Amiodarone | III (plus I, II, IV) | Ventricular tachycardia, AF refractory | 40‑60days | Thyroid dysfunction, pulmonary fibrosis, photosensitivity | Severe liver disease, iodine allergy | LFTs, TSH, pulmonary function, eye exam |
| Dofetilide | III | AF conversion/maintenance | ~10hours | QT prolongation, torsades | CrCl < 20ml/min, electrolyte imbalance | Daily ECG for 3days; renal function |
| Sotalol | III+II | AF, ventricular ectopy | ~12hours | QT prolongation, bronchospasm | Asthma, severe CKD | ECG, electrolytes, renal function |
| Flecainide | IC | Paroxysmal AF, SVT | ~12hours | Pro‑arrhythmia, visual disturbances | CAD, LV dysfunction | ECG, symptom review |
| Propafenone | IC (beta‑blocker) | AF, SVT | ~7‑10hours | Metallic taste, bradycardia | Structural heart disease | ECG, rate monitoring |
| Metoprolol | II | Rate control, post‑MI | ~3‑7hours | Fatigue, depression | Severe asthma, bradycardia | Pulse, blood pressure |
| Verapamil | IV | Rate control, hypertension | ~3‑7hours | Constipation, edema | Heart failure, severe hypotension | BP, heart rate |
| Digoxin | Cardiac glycoside | Rate control in AF with HF | ~36hours | Nausea, visual halos | AV block, hyperkalemia | Serum digoxin level, electrolytes |

How to Choose the Right Drug for You
Picking the best antiarrhythmic isn’t a one‑size‑fits‑all decision. Use the following checklist as a decision tree:
- Identify the arrhythmia type. Ventricular tachycardia usually pushes clinicians toward Amiodarone or implantable devices. Atrial fibrillation often allows several rhythm or rate options.
- Assess heart structure. If echocardiography shows reduced ejection fraction or scar tissue, avoid ClassIC agents.
- Check renal and hepatic function. Poor kidney function narrows choices to drugs with minimal renal clearance (e.g., Amiodarone, though it still needs liver monitoring).
- Consider comorbidities. Asthma favors non‑beta‑blocking agents; thyroid disease makes Amiodarone risky.
- Evaluate monitoring capacity. If you can’t commit to weekly labs or ECGs, a simpler beta‑blocker may be safer.
With these steps, you’ll have a clear picture of whether the high‑efficacy, high‑maintenance Amiodarone, or a smoother‑running alternative fits your lifestyle.
Practical Tips for Managing Amiodarone Therapy
Even if Amiodarone ends up being the right choice, you can take steps to minimize its drawbacks:
- Start low, go slow. A gradual titration reduces the risk of early pulmonary toxicity.
- Guard against thyroid swings. Keep a calendar for TSH checks every six months; an early rise may signal hypothyroidism that’s easily treatable.
- Protect your lungs. If you develop a persistent cough or shortness of breath, request a chest X‑ray or pulmonary function test right away.
- Shield your skin. Amiodarone makes you photosensitive-use sunscreen and wear sunglasses.
- Stay hydrated. Adequate fluid intake supports liver clearance.
When to Switch Away from Amiodarone
There are clear red flags that signal it’s time to look for an alternative:
- Documented pulmonary fibrosis on imaging. \n
- TSH rises above 10µIU/mL despite replacement therapy.
- Elevated liver enzymes >3× upper limit of normal.
- Persistent visual disturbances or corneal deposits affecting vision.
In these scenarios, discuss options like Dofetilide (if kidney function is adequate) or a beta‑blocker for rate‑only control. Transitioning should be done under close supervision to avoid rebound arrhythmias.
Bottom Line
Amiodarone remains a heavyweight champion for life‑threatening arrhythmias, but the “price” is its long‑term toxicity and monitoring burden. Modern practice often starts with safer, short‑acting agents-Dofetilide, Sotalol, Flecainide, or Propafenone-reserving Amiodarone for cases where those drugs fail or where ventricular rhythm control is critical.
Ask your cardiologist about your specific heart condition, how often you can get labs, and what side‑effects you’re most comfortable monitoring. Armed with that information, you can choose a therapy that balances effectiveness with quality of life.
Frequently Asked Questions
Can I take Amiodarone and a beta‑blocker together?
Yes, many patients use a beta‑blocker like Metoprolol to control heart rate while Amiodarone maintains rhythm. The combo can increase the risk of bradycardia, so regular pulse checks are essential.
How long does it take for Amiodarone to leave my system?
Because its half‑life ranges from 40 to 60 days, it may take 6‑9 months for the drug to clear fully after stopping. Some tissue stores linger even longer.
Is Dofetilide safe for someone with mild kidney disease?
Dofetilide dosing is adjusted based on creatinine clearance. Patients with CrCl>40ml/min usually tolerate standard doses, but anyone below 20ml/min should avoid it.
Why does Amiodarone cause thyroid problems?
Amiodarone contains iodine and can both block thyroid hormone synthesis (causing hypothyroidism) and trigger excess release (causing hyperthyroidism). Regular TSH testing catches these changes early.
What’s the difference between rate control and rhythm control?
Rate control slows the heart’s beating speed but doesn’t restore normal electrical patterns. Rhythm control aims to convert the heart back to its regular sinus rhythm. The choice depends on symptom severity, underlying disease, and medication tolerance.





Zackery Brinkley
September 29, 2025 AT 16:29Hey, I totally get how scary the side‑effects list for amiodarone can look. If you’re already on it, try scheduling those liver and thyroid checks well in advance so they don’t feel like a surprise. Staying on top of your labs makes the whole thing feel a lot less overwhelming.
Luke Dillon
October 3, 2025 AT 17:42Just a friendly heads‑up: if you have any history of lung issues, let your doc know early. A quick chest X‑ray right after starting amiodarone can catch tiny changes before they become a real problem.
Elle Batchelor Peapell
October 7, 2025 AT 18:55When you look at the landscape of rhythm control, amiodarone sits like a heavyweight champion that carries a massive belt of side‑effects. Its ability to tame both ventricular tachycardia and atrial fibrillation is unrivaled, yet that same power brings a cascade of concerns that echo through every organ system. Think of the thyroid as a delicate orchestra; the iodine load from amiodarone can either silence the strings with hypothyroidism or crank them up to a chaotic hyper‑thyroid crescendo. The lungs, too, can become a silent battleground, where subtle interstitial changes creep in unnoticed until a cough or dyspnea forces a CT scan. Your liver, the body's chemical factory, bears the brunt of repeated dosing, and elevations in transaminases can be the first whisper of trouble. Then there’s the eye-corneal deposits that may cause a halo effect around lights, often dismissed as merely a visual quirk. All these risks underscore why regular monitoring is non‑negotiable; it’s the only way to keep the drug’s benefits from eclipsing its dangers. Yet, for many patients whose arrhythmias are life‑threatening and refractory to other agents, amiodarone remains the only viable lifeline. In that narrow window, the trade‑off becomes a calculated gamble rather than an outright danger. What matters most is a clear dialogue between patient and physician, laying out the timeline for labs, the signs that demand immediate attention, and a contingency plan for switching therapies if toxicity spikes. In practice, this often means a disciplined schedule: TSH and liver enzymes every six months, pulmonary function tests annually, and an eye exam at least once a year. For those who can commit to that regimen, amiodarone can be a salvation; for others, the safer, short‑acting alternatives might be a better road. So while the drug’s presence on the market may feel daunting, its strategic use-paired with vigilant follow‑up-can transform a potential liability into a life‑saving tool.
Jeremy Wessel
October 11, 2025 AT 20:09Amiodarone works broad but watch thyroid liver lungs.
Laura Barney
October 15, 2025 AT 21:22Let’s paint a picture: imagine your heart as a bustling city and amiodarone as the traffic cop who can stop any rogue driver, but he also blocks the sunshine, causing the streets to get a bit gloomy. If you have a sun‑loving soul, maybe a sleeker car like flecainide or sotalol would keep the streets lively without the shadows.
Jessica H.
October 19, 2025 AT 22:35From a strictly clinical perspective, the author neglects to emphasize that the long half‑life of amiodarone imposes a significant risk of delayed toxicity. Moreover, the recommendation to “start low, go slow” is overly simplistic; dose titration must be individualized based on serial pulmonary function tests and thyroid panels, not merely anecdotal thresholds.
Tom Saa
October 23, 2025 AT 23:49Considering the balance of efficacy and toxicity, one could argue that the piece glosses over the nuanced decision‑making required when comorbidities intersect. Still, the core message about monitoring remains solid.
John Magnus
October 28, 2025 AT 00:02From a pharmacodynamic standpoint, amiodarone’s multi‑channel blockade confers a unique antiarrhythmic profile, yet its lipophilicity results in profound tissue sequestration. Clinicians must weigh the risk of QT‑prolongation against the necessity for ventricular arrhythmia suppression, employing telemetry and serial ECGs to mitigate torsades de pointes risk.
Marc Clarke
November 1, 2025 AT 01:15Honestly, the table’s layout is pretty helpful and the side‑effect summary hits the nail on the head; a quick glance gives you the gist without scrolling through dense prose.
Ted Whiteman
November 5, 2025 AT 02:29It’s all just hype.
Vivian Yeong
November 9, 2025 AT 03:42The article oversimplifies the decision algorithm; real‑world practice demands more granular risk stratification.
suresh mishra
November 13, 2025 AT 04:55Check renal function before picking a potassium‑blocker; dose adjusts accordingly.
Cassidy Strong
November 17, 2025 AT 06:09Note: The phrase “long‑term monitoring requirements” should be hyphenated; also, “renal function narrows choices” would read clearer with a comma before “to drugs”.
Danielle Spence
November 21, 2025 AT 07:22People who think amiodarone is a miracle drug clearly haven’t bothered to read the fine print on organ toxicity. If you’re comfortable with half‑life measured in months, go ahead, but most of us would rather avoid a medication that makes the thyroid act like a roller coaster.
Dhanu Sharma
November 25, 2025 AT 08:35Totally get the frustration; the drug’s efficacy is impressive, but the monitoring schedule feels like a full‑time job.
Edward Webb
November 29, 2025 AT 09:49Indeed, balancing therapeutic benefit against the logistical burden of serial labs is a pivotal consideration. Patients with limited access to healthcare facilities may find the regimen impractical, prompting a preference for agents with shorter half‑lives and less stringent follow‑up.
Snehal Suhane
December 3, 2025 AT 11:02Oh, sure, let’s just ignore the fact that amiodarone’s half‑life is practically a lifetime in the making-because why would anyone care about practicality?
Anoop Choradia
December 7, 2025 AT 12:15One must contemplate, with the utmost seriousness, whether the pharmaceutical conglomerates have not subtly engineered the narrative surrounding amiodarone to perpetuate a shadow of dependence among clinicians, thereby ensuring an uninterrupted supply chain that benefits obscure stakeholders beyond the immediate medical community.
bhavani pitta
December 11, 2025 AT 13:29In the grand theatre of cardiology, amiodarone assumes the role of both hero and antagonist-saving lives on the battlefield while silently carving its own tragic saga upon the body.