When you hear "metabolic syndrome," it might sound like a fancy medical term-but what it really means is your body is sending out warning signs. And those signs? They show up in three places you can measure right now: your waist, your blood triglycerides, and your fasting glucose. If you’ve been told you have prediabetes, or your doctor mentioned your cholesterol is off, or your pants don’t fit like they used to-this is why.
What Exactly Is Metabolic Syndrome?
Metabolic syndrome isn’t one disease. It’s a cluster of three or more risk factors that pile up together and dramatically raise your chance of heart disease, stroke, and type 2 diabetes. Think of it like a domino effect: one problem triggers another, and soon you’re facing a whole cascade of health issues.
The big three? Abdominal fat (measured by waist size), high triglycerides, and elevated blood sugar. Add in high blood pressure or low HDL (the "good" cholesterol), and you’ve got the full picture. According to the National Heart, Lung, and Blood Institute, about 34.7% of U.S. adults have metabolic syndrome. That’s more than one in three. And it’s not just older people-rates are climbing fast in people in their 30s and 40s.
Why Waist Size Matters More Than You Think
It’s not just about looking heavier. It’s about where the fat is stored. Belly fat-especially the kind that wraps around your organs-isn’t just padding. It’s active tissue that releases chemicals that mess with how your body uses insulin.
The numbers matter:
- Men: waist over 40 inches (102 cm)
- Women: waist over 35 inches (88 cm)
These aren’t arbitrary numbers. Research from Circulation found that every extra 4 inches (10 cm) around your waist increases your risk of heart disease by 10%. And it’s not just about weight-someone can have a normal BMI and still have dangerous belly fat. That’s called "normal-weight obesity," and it’s more common than you’d think.
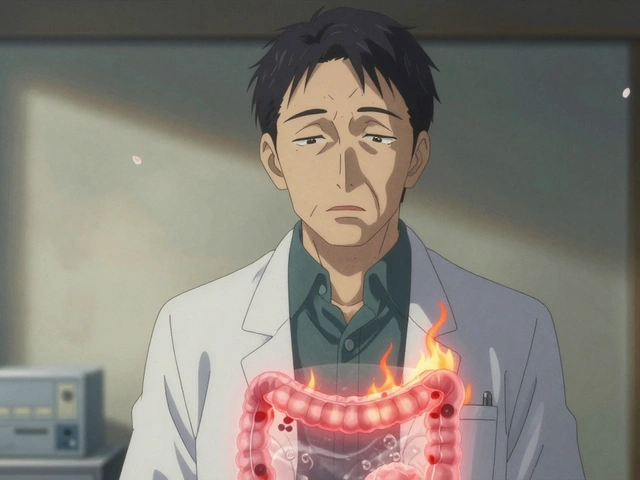
Why does this happen? Fat cells in your abdomen pump out inflammatory signals like tumor necrosis factor-alpha and resistin. These chemicals block insulin from doing its job. That’s the first domino.
Triglycerides: The Hidden Lipid Threat
Triglycerides are a type of fat in your blood. When you eat more calories than your body can use right away-especially from sugar and refined carbs-your liver turns the excess into triglycerides and stores them in fat cells.
Normal levels? Below 150 mg/dL. If you’re over that, you’re in the danger zone. But here’s the catch: levels above 200 mg/dL don’t just mean you have metabolic syndrome-they independently raise your risk of heart attack and stroke, even if your LDL cholesterol is fine.
How is this connected to your waist? When insulin resistance kicks in, your liver starts overproducing very-low-density lipoprotein (VLDL), which carries triglycerides into your bloodstream. So belly fat → insulin resistance → high triglycerides. It’s a direct line.
And it gets worse. High triglycerides themselves make insulin resistance worse. That’s called lipotoxicity-fat molecules clogging up muscle and liver cells so they can’t respond to insulin anymore. You’re stuck in a loop.

Glucose Control: The Early Warning Sign
Your fasting blood sugar should be under 100 mg/dL. If it’s between 100 and 125, you have prediabetes. That’s not just a label-it’s your body screaming that insulin isn’t working.
When your muscles and liver stop responding to insulin, glucose can’t get into your cells to be used for energy. So it stays in your blood. Your pancreas tries to compensate by pumping out more insulin. Eventually, it burns out. That’s when type 2 diabetes kicks in.
The numbers are scary: people with prediabetes have a 5-10% chance each year of developing full-blown diabetes. The Diabetes Prevention Program showed that with lifestyle changes-losing 5-7% of body weight and getting 150 minutes of exercise a week-you can cut that risk by 58%. That’s more effective than any pill.
The Real Culprit: Insulin Resistance
Every single piece of metabolic syndrome ties back to one thing: insulin resistance. It’s not caused by eating too much fat. It’s caused by too much sugar, too many refined carbs, too little movement, and too much stress-all of which lead to fat building up in your belly.
Dr. Robert Eckel, a leading expert from the American Heart Association, put it simply: "Abdominal obesity is the trigger. Insulin resistance is the engine. Everything else follows."
That’s why fixing your waist size is the most powerful thing you can do. Losing just 5-10% of your body weight can:
- Lower triglycerides by 20-50%
- Improve fasting glucose by 20-40%
- Reduce blood pressure by 5-10 mm Hg
- Boost HDL cholesterol
And you don’t need to lose 50 pounds. Even 10-15 pounds can reverse metabolic syndrome for many people.
What You Can Do Right Now
You don’t need a miracle. You need a plan. Here’s what actually works, based on real studies:
1. Cut Added Sugar and Refined Carbs
That soda, the white bread, the cereal, the pastries-they’re all turning into triglycerides and spiking your blood sugar. The American Heart Association recommends limiting added sugar to less than 10% of your daily calories. For most people, that’s about 12 teaspoons a day. Most Americans consume 20+.
2. Move Every Day
You don’t need to run a marathon. Just 30 minutes of brisk walking five days a week cuts insulin resistance. Strength training twice a week helps even more-muscle burns glucose, even at rest.
3. Eat Real Food
Focus on vegetables, lean proteins, nuts, seeds, legumes, and healthy fats like olive oil and avocado. The PREDIMED trial showed that a Mediterranean-style diet reduced heart events by 30% in people with metabolic syndrome.
4. Sleep and Stress Matter
Chronic stress raises cortisol, which drives belly fat storage. Poor sleep messes with hunger hormones and makes you crave sugar. Aim for 7-8 hours of quality sleep. If you’re stressed, try breathing exercises, walking in nature, or yoga-even 10 minutes a day helps.
5. Know Your Numbers
Get your waist measured. Ask for a fasting lipid panel and fasting glucose. Don’t wait for symptoms. If you’re over 40, overweight, or have a family history of diabetes or heart disease, get checked now.

When Medication Might Help
Lifestyle is always the first step. But sometimes, you need a little help.
- Metformin is the go-to for prediabetes. It improves insulin sensitivity and lowers glucose without causing weight gain.
- Omega-3 fatty acids (4 grams daily) are prescribed if triglycerides are above 500 mg/dL.
- ACE inhibitors or ARBs may be used if blood pressure is high-they also help protect the kidneys, which are often damaged early in metabolic syndrome.
But here’s the truth: no pill replaces weight loss. Medications manage symptoms. Lifestyle fixes the root cause.
What’s Next? The Future of Metabolic Health
Researchers are now looking beyond the five traditional criteria. A new tool called the TyG index-calculated from your fasting triglycerides and glucose-is showing promise as a simple, cheap way to spot insulin resistance before full-blown metabolic syndrome develops.
And there’s exciting work on the gut microbiome. Scientists have found specific gut bacteria patterns linked to metabolic syndrome. In the future, personalized probiotics or dietary tweaks based on your gut flora could become part of treatment.
But for now? The solution is simple, proven, and available to everyone: lose belly fat, lower triglycerides, and bring glucose down. You don’t need a fancy device or expensive supplement. Just food, movement, sleep, and consistency.
Don’t Wait for a Diagnosis
If your waist is creeping up, your triglycerides are over 150, or your fasting glucose is above 95-you’re already on the path. But you’re not doomed. You’re in the window where change still works.
Metabolic syndrome isn’t a life sentence. It’s a wake-up call. And you have more power to reverse it than you think.





Marilyn Ferrera
January 1, 2026 AT 17:10Waist size isn't just a number-it's a silent scream from your liver, your pancreas, your cells begging for mercy.
Every inch past 40 for men? That's not fat. That's inflammation with a pulse.
I used to think 'healthy weight' meant the scale. Now I know-it's the tape measure that doesn't lie.
And glucose? It's not about willpower. It's about biology being hijacked by sugar.
One soda a day. For ten years. That's not a habit. That's a slow-motion suicide.
But here's the hope: reverse it? Yes. Not with drugs. With discipline. With food that doesn't come in a box.
Metformin helps-but it doesn't fix the root. Only you can do that.
Stop waiting for a diagnosis. Your body's already texting you. Read the messages.
Branden Temew
January 2, 2026 AT 00:52So let me get this straight-we’ve got a syndrome named after a buzzword, and the cure is… eating less cake? Shocking.
Next you’ll tell me breathing oxygen is ‘clinically proven’ to reduce mortality.
But hey-I’ll take ‘eat veggies, walk more’ over another pill that costs $500 a month and makes me pee like a racehorse.
Still… why does the medical industry need a 2000-word essay to say ‘stop being lazy’?
Also-why is ‘normal-weight obesity’ a thing? Sounds like a dystopian dating profile.
Frank SSS
January 3, 2026 AT 22:45Look, I get it-fat around the middle is bad. But let’s be real: most people don’t care until their pants split in public.
I’ve seen guys with 38-inch waists who run marathons and eat kale. And I’ve seen 220-pound guys with 32-inch waists who live on pizza rolls.
Waist size? Maybe. But it’s still a proxy. A noisy, oversimplified proxy.
And don’t even get me started on ‘fasting glucose.’ I fasted for 14 hours and still got a 108 because I had a protein bar at 9 PM.
Doctors love metrics. But biology’s messy. And so are we.
Still… if cutting soda and walking helps? Fine. I’ll do it. But don’t sell me this as science. It’s common sense with a lab coat.
Paul Huppert
January 5, 2026 AT 05:08I really appreciate how this breaks it down without jargon.
I had no idea belly fat was actively messing with insulin like that.
I thought triglycerides were just ‘bad cholesterol’-but now I see they’re a direct result of sugar overload.
My dad had metabolic syndrome-he lost 18 pounds just by ditching soda and walking after dinner.
He didn’t need meds. Just consistency.
It’s funny… the solution’s always been simple. It’s the world around us that made it hard.
Thanks for the clarity.
Hanna Spittel
January 5, 2026 AT 19:34THEY KNOW. THEY KNOW WHAT’S HAPPENING. 🤫
Why is this only being discussed now? 🤔
Sugar was pushed by corporations for DECADES. 🍭
And now they want you to ‘eat better’ like it’s your fault? 😒
Also-metformin? That’s a diabetes drug. But they give it to healthy people now? 👀
Who’s profiting? 🕵️♀️
Also-gut bacteria? I think my colon is a cult. 🦠
Brady K.
January 6, 2026 AT 22:39Let’s cut through the noise: metabolic syndrome isn’t a medical condition-it’s a societal failure.
We’ve engineered a world where movement is optional, food is engineered to be addictive, and sleep is a luxury.
And then we blame the individual for ‘not trying hard enough’?
Here’s the truth: if you live in a food desert, work two jobs, and sleep 5 hours a night-your body is doing its best to survive.
‘Lose 10 pounds’? Sure. But only if you’ve got time, money, and access to real food.
Otherwise? You’re just playing Russian roulette with your pancreas.
Stop preaching. Start fixing systems.
And yes-I’ve reversed mine. But I had the privilege to do so.
Kayla Kliphardt
January 8, 2026 AT 16:48I didn’t know waist size was such a strong predictor.
I’ve always focused on BMI.
My doctor never measured my waist. Just said ‘you’re overweight.’
I just checked-41 inches.
…I’m going to start walking after dinner.
Thanks for making me pay attention.
John Chapman
January 9, 2026 AT 05:20Bro. I lost 22 pounds in 4 months. Just cut sugar. Walked 6k steps a day. Slept 7 hours.
Triglycerides dropped from 280 to 110.
Fasting glucose went from 118 to 87.
Waist went from 42 to 34.
No meds. No shakes. Just food and movement.
You can do this. I’m not special.
Start today. Not Monday.
🔥
Urvi Patel
January 10, 2026 AT 11:39