Chronic acid reflux isn’t just a nuisance-it’s a silent warning sign that could lead to esophageal cancer. If you’ve had heartburn for five years or more, especially if you’re a man over 50, overweight, or a smoker, your risk isn’t just higher-it’s significantly elevated. The truth is, most people with GERD never develop cancer, but the ones who do often ignore the early signals until it’s too late. Esophageal adenocarcinoma, the most common type linked to GERD, has seen an 850% increase since the 1970s, and the main driver is simple: more people have long-term acid reflux, and more are obese.
How GERD Turns Into Cancer
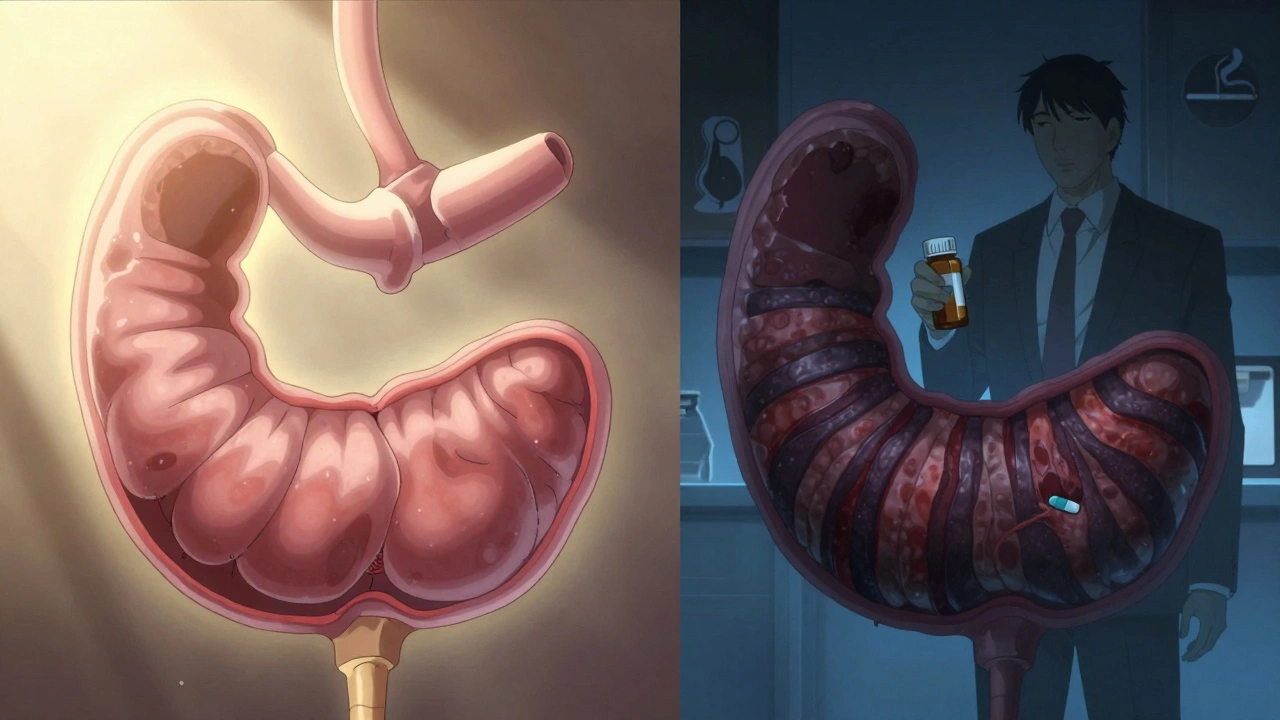
Your esophagus isn’t meant to handle stomach acid. Every time acid backs up, it burns the lining. Over time, your body tries to protect itself by changing the cells there. Instead of the normal flat cells, they start looking like stomach lining. That’s called Barrett’s esophagus. It’s not cancer. But it’s the only known precursor to esophageal adenocarcinoma. Once Barrett’s develops, the risk of cancer climbs-but slowly. Only about 0.2% to 0.5% of people with Barrett’s develop cancer each year. That sounds low, but when you’re talking about millions of people with GERD, even a small percentage adds up.
Studies show that people with GERD for five or more years are five times more likely to develop Barrett’s esophagus than those without it. And if you’re having symptoms weekly, your risk of esophageal cancer jumps sevenfold. The key isn’t how bad the heartburn feels-it’s how long it’s been going on. Even mild reflux, if it lasts a decade or more, can trigger the same cellular changes.
Who’s Most at Risk?
Not everyone with GERD is equally at risk. Certain factors stack the deck. The biggest ones:
- Male sex: Men are 3 to 4 times more likely than women to develop esophageal adenocarcinoma.
- Age over 50: 90% of cases happen in people over 55. New or worsening reflux after 50 is a red flag.
- White, non-Hispanic ethnicity: White Americans have three times the rate of adenocarcinoma compared to Black Americans.
- Obesity: A BMI over 30 doubles or triples your risk. Fat around the abdomen pushes stomach contents upward.
- Smoking: Current or past smokers have 2 to 3 times the risk. The damage from tobacco compounds the acid damage.
- Family history: If a close relative had esophageal cancer, your risk goes up.
Having just one or two of these doesn’t mean you’ll get cancer. But if you’re a 60-year-old white man with a 15-year history of GERD, a BMI of 32, and you used to smoke? You’re in the high-risk group. And you should be talking to a doctor about an endoscopy.
The Red Flags That Demand Action
Most esophageal cancers are caught too late-75% are diagnosed after they’ve spread. Why? Because early symptoms are easy to dismiss. But these signs aren’t normal:
- Dysphagia: Feeling like food is stuck in your chest or throat. It usually starts with solids, then moves to liquids. This is present in 80% of diagnosed cases.
- Unexplained weight loss: Losing 10 pounds or more in six months without trying. No diet, no extra exercise-just weight gone.
- Chronic hoarseness or cough: A voice that won’t clear up or a cough that lasts more than two weeks, especially if you don’t smoke.
- Food impaction: Food gets stuck and you can’t get it down, even after drinking water.
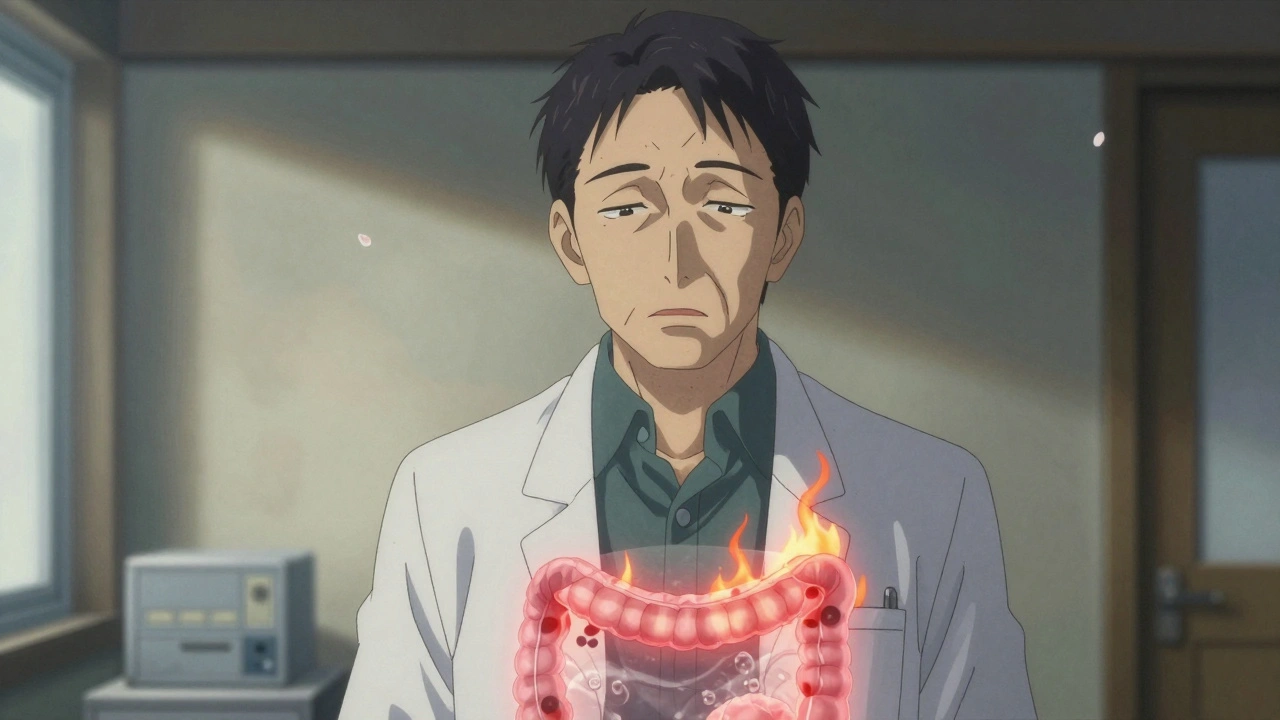
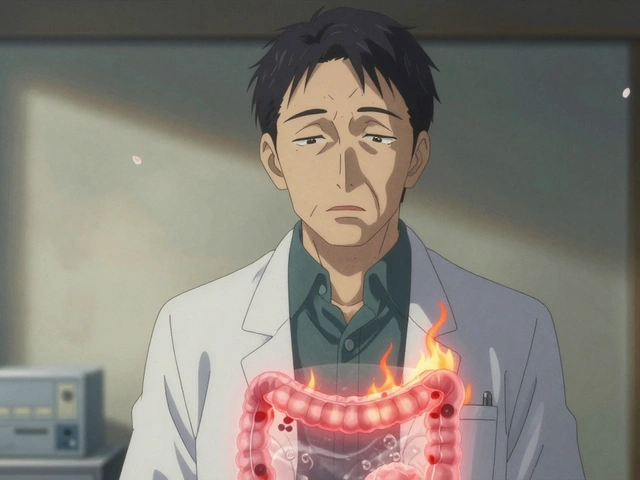
- Heartburn that won’t quit: If you’re having it more than twice a week for five or more years, that’s not just bad digestion-it’s a warning.
These aren’t vague symptoms. They’re measurable, documented signals. If you have one of these, especially with multiple risk factors, don’t wait. Get an endoscopy. It’s a simple, quick procedure. A scope goes down your throat, and the doctor looks for Barrett’s esophagus or early cancer. If they find it early, the survival rate jumps from 21% to 50-60%.
What You Can Do to Lower Your Risk
It’s not all doom and gloom. You have control over many of the factors.
- Quit smoking: Your risk drops by half within 10 years of quitting.
- Lose weight: Shedding just 5-10% of your body weight cuts GERD symptoms by 40% in obese people.
- Limit alcohol: Stick to one drink a day for women, two for men. Heavy drinking raises a different type of esophageal cancer, but it still adds risk.
- Take PPIs as prescribed: If you’ve been diagnosed with Barrett’s esophagus, consistent use of proton pump inhibitors (like omeprazole or esomeprazole) for five years reduces cancer risk by 70%.
- Get screened: If you’re a white male over 50 with chronic GERD and two other risk factors, the American College of Gastroenterology recommends an upper endoscopy. Yet only 13% of high-risk people get one. Don’t be in that group.
There’s also new tech on the horizon. A pill-sized sponge called the Cytosponge, which you swallow and then pull back up, collects cells from your esophagus. It’s less invasive than an endoscopy and found Barrett’s with nearly 80% accuracy in trials. It’s not standard yet, but it’s coming.
Why Early Detection Saves Lives
Esophageal cancer kills about 16,780 people in the U.S. each year. The five-year survival rate is just 21%. But that number is misleading. If caught early-before it spreads beyond the esophagus-the survival rate climbs to 50-60%. That’s a huge difference. And the only way to catch it early is to screen people who are at risk.
Doctors aren’t being alarmist. They’re being practical. GERD is common. Barrett’s is rare. Cancer from it is rarer still. But when you have the perfect storm-long-term reflux, male gender, age, obesity, smoking-the math changes. The risk isn’t theoretical. It’s in the data. And the fix? It’s simple: know your risk, watch for red flags, and get checked.
Don’t wait until swallowing hurts. Don’t assume weight loss is just stress. Don’t think your heartburn is "just part of aging." These are not normal. They’re signals. And if you’re in a high-risk group, ignoring them could cost you your life.
Is GERD the same as occasional heartburn?
No. Occasional heartburn-once a month or less-is common and usually harmless. GERD is chronic acid reflux that happens at least twice a week for several weeks or longer. It’s diagnosed when symptoms persist despite over-the-counter treatments or when they start affecting your sleep, eating, or daily life. Long-term GERD (five+ years) is what raises cancer risk.
Can I get Barrett’s esophagus without having GERD symptoms?
Yes. About 10-20% of people with Barrett’s esophagus have no noticeable heartburn or reflux. This is called "silent GERD." The acid damage still happens, especially at night or when lying down. That’s why screening isn’t just for people who feel bad-it’s for those with risk factors, even if they don’t have classic symptoms.
Does taking antacids or PPIs prevent esophageal cancer?
They help, but they’re not a guarantee. PPIs reduce acid exposure, which lowers the chance of Barrett’s developing or worsening. For people already diagnosed with Barrett’s, taking PPIs consistently for five years cuts cancer risk by 70%. But if you stop taking them, the protection fades. They’re part of management, not a cure. Lifestyle changes and screening are still essential.
Should I get an endoscopy if I have GERD but no other risk factors?
Generally, no. Most guidelines recommend endoscopy only if you’re over 50, male, white, and have chronic GERD plus at least two other risk factors (like obesity or smoking). If you’re younger, female, and have mild GERD with no other risks, your cancer risk is very low. But if you develop new red flag symptoms-like trouble swallowing or unexplained weight loss-you should get checked regardless of your risk profile.
Is esophageal cancer hereditary?
Not directly. But having a close family member (parent, sibling) with esophageal cancer does increase your risk. This could be due to shared genetics, lifestyle habits, or both. If you have a family history, talk to your doctor about earlier or more frequent screening, even if you’re under 50.
Can I reverse Barrett’s esophagus?
In some cases, yes. With consistent PPI use, weight loss, and quitting smoking, the abnormal cells can regress back to normal lining in about 10-20% of patients. Even if it doesn’t fully reverse, controlling acid exposure slows or stops progression to cancer. Regular endoscopic monitoring is still needed because the risk doesn’t disappear.





Arun kumar
December 3, 2025 AT 05:46man i had heartburn for like 8 years and never thought twice about it. guess i was lucky. now i’m thinking maybe i should’ve gotten checked. kinda scary how quietly this stuff creeps up.
Zed theMartian
December 4, 2025 AT 07:44Oh wow. Another ‘your body is a fragile china doll’ PSA from the medical-industrial complex. Let me guess - next they’ll tell us breathing increases lung cancer risk because ‘acidic air’? This isn’t medicine, it’s fear marketing dressed in lab coats. I’ve had GERD since college. I’m 58. Still alive. Still digesting tacos. And no, I won’t be swallowing a pill for 5 years to ‘prevent’ something that statistically won’t happen to me.
ATUL BHARDWAJ
December 5, 2025 AT 09:07GERD common. Cancer rare. But silence kills. Get checked if risk factors match. Simple.
Steve World Shopping
December 6, 2025 AT 04:26Pathophysiological progression from chronic gastroesophageal reflux to metaplastic Barrett’s epithelium represents a classic example of inflammation-driven carcinogenesis. The molecular cascade involving NF-kB, COX-2, and oxidative DNA damage is well-documented in peer-reviewed literature. Yet, public health messaging remains tragically reductive. You’re not just ‘having heartburn’ - you’re undergoing epigenetic reprogramming of your esophageal mucosa. If you’re a male over 50 with abdominal adiposity and a smoking history, you’re not ‘at risk’ - you’re in a high-risk phenotypic cohort. Screening isn’t optional. It’s a biostatistical imperative.
Rebecca M.
December 6, 2025 AT 15:34Oh great. So now I’m supposed to feel guilty for loving my midnight pizza and wine? And also for being a woman? Wait - no, I’m safe because I’m not white and male? Thanks for that, science. I’ll just keep ignoring my acid reflux while sipping chamomile tea and pretending I’m not a demographic target for corporate oncology.
Jay Everett
December 8, 2025 AT 04:55Guys. I’m a nurse. I’ve seen this play out. A guy, 62, never thought twice about heartburn. Thought it was ‘just stress’. Lost 30 lbs in 4 months, said he was ‘eating less’. Then he couldn’t swallow his own saliva. Endoscopy found stage 3. He’s gone now. His wife cried in my office for an hour. This isn’t fearmongering. It’s *fact*. PPIs aren’t magic. Weight loss isn’t a trend. Quitting smoking? One of the best things you’ll ever do for your body. Do it. Not for the blog. For you. ❤️
Jack Dao
December 8, 2025 AT 19:18It’s pathetic how people treat their bodies like disposable electronics. ‘I’ll just take an antacid’ - yeah, until your esophagus turns into a science experiment. You don’t get to ignore biology because you’re too lazy to change your diet or quit smoking. And don’t even get me started on people who think ‘natural remedies’ fix Barrett’s. It’s not a Spotify playlist. It’s your damn lining. Get screened. Or don’t. But don’t act surprised when your life ends early because you thought you were invincible.
Laura Baur
December 10, 2025 AT 09:08I find it fascinating how this post reduces human health to a checklist of demographic checkboxes - white, male, over 50, obese, smoker - as if these are moral failings rather than complex intersections of socioeconomic status, food deserts, genetic predisposition, and lack of access to preventative care. You talk about ‘risk factors’ like they’re personal choices, but for many, ‘losing weight’ means choosing between rent and groceries. ‘Quit smoking’ is easier said than done when your community has no mental health support and nicotine replacement is $50 a week. The real red flag isn’t GERD - it’s a healthcare system that blames individuals for systemic failures. Screening is good, yes - but equity is better.
dave nevogt
December 11, 2025 AT 12:07I’ve been reading this slowly. It’s heavy. Not because it’s scary - but because it’s true. I’m 57. Had GERD since I was 38. Never thought it was serious. I lost weight last year. Quit smoking. Started taking PPIs. I don’t feel like a ‘high-risk’ person. I just feel like someone who finally listened. I got my endoscopy last month. No Barrett’s. But I’m still going back every two years. Not because I’m afraid. Because I want to be around for my grandkids. That’s all.
Ella van Rij
December 11, 2025 AT 17:12So… if I’m a 45-year-old black woman with GERD and a BMI of 28… am I just… safe? Like, can I go back to eating nachos and ignoring my throat burn? Because if so, I’m gonna do it. Also, I think ‘silent GERD’ is just code for ‘you’re not complaining loud enough’.
Lynn Steiner
December 13, 2025 AT 15:48They’re coming for us. First they take our burgers, then our wine, then our sleep. Next thing you know, they’ll be scanning our throats in the grocery store. I’m not getting an endoscopy. I’d rather die on my terms than let some doctor stick a camera down my throat because I ate pizza on a Friday. I’m not a statistic. I’m a person. And I refuse to be terrorized by medical jargon.
Alicia Marks
December 15, 2025 AT 03:40You got this. Small changes = big results. Start with one thing - maybe skip the late-night snacks. Or drink water after meals. You don’t have to fix everything today. Just start. And if you’re scared? Talk to your doctor. You’re not alone.
Paul Keller
December 15, 2025 AT 21:47Let me be clear: the data is unequivocal. The 850% rise in esophageal adenocarcinoma since the 1970s correlates directly with the rise in obesity rates and the normalization of chronic acid reflux as a ‘lifestyle inconvenience.’ This is not hyperbole - it is epidemiology. The Cytosponge is not a gimmick; it is a paradigm shift in screening accessibility. If you are in a high-risk cohort, the cost of inaction is not merely medical - it is existential. I am not advocating for panic. I am advocating for agency. Knowledge is power. Action is responsibility. And silence? Silence is the most expensive commodity in healthcare.