Diuretic Selection Assistant
Your Clinical Scenario
Recommendations
If you’ve ever heard of Furosemide, you probably know it’s a powerful diuretic that doctors rely on to pull excess fluid out of the body. Whether you’re managing heart failure, kidney disease, or high blood pressure, you’ll quickly run into the question: Is Furosemide the best choice, or should you consider another option?
What Is Furosemide?
Furosemide is a loop diuretic that blocks the Na⁺‑K⁺‑2Cl⁻ transporter in the thick ascending limb of the loop of Henle. By stopping sodium and chloride from being re‑absorbed, it forces the kidneys to dump more water into the urine. The drug is sold under brand names like Lasix and UniDiur, and it entered the market in the early 1960s.
How a Loop Diuretic Works
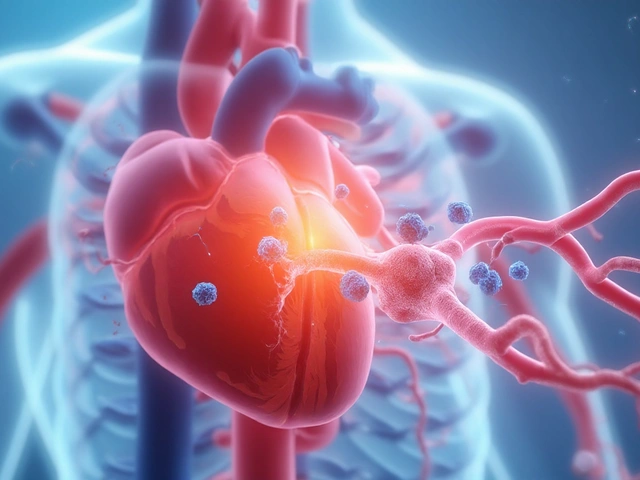
Loop diuretics, including Furosemide, are the most potent class of water‑removing drugs. They act early in the nephron, so the effect kicks in within 30‑60 minutes and can last up to 6‑8 hours. This rapid, strong diuresis makes them the go‑to for acute pulmonary edema or severe fluid overload.
Common Alternatives to Furosemide
Not every patient tolerates Furosemide, and sometimes clinicians need a different profile of action, side‑effects, or cost. Below are the most frequently used alternatives, each with its own niche.
Hydrochlorothiazide
Hydrochlorothiazide belongs to the thiazide class. It works farther down the nephron, at the distal convoluted tubule, slowing sodium re‑absorption there. The result is a milder diuresis that’s ideal for long‑term blood‑pressure control but less effective for rapid fluid removal.
Torsemide
Torsemide is another loop diuretic, often marketed as Demadex. It shares the same mechanism as Furosemide but has a longer half‑life (about 6‑8 hours) and a more predictable oral absorption, which can be useful for patients who struggle with the short‑acting nature of Furosemide.
Bumetanide
Bumetanide (Bumex) is one of the most potent loops-about 40 times more powerful than Furosemide on a per‑milligram basis. Because the dose is tiny, it’s sometimes preferred when high potency is needed without large tablet sizes.
Metolazone
Metolazone straddles the line between thiazide‑type and loop‑type activity. It works in the distal tubule but retains some efficacy even when kidney function is reduced, making it a useful add‑on for chronic kidney disease patients.
Ethacrynic acid
Ethacrynic acid is the only non‑sulfonamide loop diuretic, which matters for patients allergic to sulfa drugs. It’s less commonly used because it can cause hearing loss at high doses, but it’s a lifesaver when other loops are contraindicated.

Head‑to‑Head Comparison
| Drug | Class | Typical Oral Dose | Onset | Duration | Key Side Effects | Average US Cost (30‑day supply) |
|---|---|---|---|---|---|---|
| Furosemide | Loop | 20‑80 mg | 30‑60 min | 6‑8 h | Hypokalemia, ototoxicity (high doses), dehydration | $10‑$15 |
| Hydrochlorothiazide | Thiazide | 12.5‑50 mg | 2‑4 h | 12‑24 h | Hyponatremia, hyperuricemia, photosensitivity | $4‑$8 |
| Torsemide | Loop | 5‑20 mg | 30‑60 min | 12‑14 h | Similar to Furosemide but less ototoxic; may cause rash | $12‑$18 |
| Bumetanide | Loop | 0.5‑2 mg | 30‑60 min | 4‑6 h | Hypokalemia, ototoxicity (rare) | $15‑$22 |
| Metolazone | Thiazide‑like | 2.5‑10 mg | 2‑4 h | 12‑24 h | Electrolyte imbalance, gout flare | $8‑$12 |
| Ethacrynic acid | Loop (non‑sulfonamide) | 25‑200 mg | 30‑60 min | 6‑8 h | Hearing loss, tinnitus, electrolyte loss | $20‑$30 |
Choosing the Right Diuretic - Quick Checklist
- Speed of diuresis needed? For emergencies, pick a short‑acting loop like Furosemide or Bumetanide.
- Kidney function? Metolazone works better when GFR < 30 mL/min; most loops lose potency.
- Allergy to sulfa? Ethacrynic acid is the safe non‑sulfonamide alternative.
- Cost constraints? Hydrochlorothiazide and generic Furosemide are the cheapest options.
- Long‑term blood‑pressure control? Thiazides (Hydrochlorothiazide) are preferred.
- Risk of hearing loss? Avoid high‑dose Furosemide or Bumetanide; consider Torsemide.
Potential Pitfalls & How to Avoid Them
Even the right drug can cause trouble if you ignore a few practical steps.
- Never start a loop diuretic without checking serum potassium. Low potassium can trigger dangerous arrhythmias.
- If you’re on a thiazide, watch for gout flare‑ups. Keep uric acid levels in mind.
- Stay hydrated, but don’t over‑drink. Excess water can blunt the drug’s effect and increase the risk of hyponatremia.
- Monitor weight daily when treating heart‑failure patients. A sudden 2‑kg jump often means the diuretic isn’t doing enough.
- Talk to your pharmacist about drug interactions. NSAIDs, for instance, can blunt the effect of most diuretics.
Bottom Line
Furosemide remains the heavyweight champion for rapid fluid removal, but it isn’t a one‑size‑fits‑all. If you need a gentler, long‑acting approach, a thiazide like Hydrochlorothiazide might be better. When sulfa allergies or specific potency needs come into play, Torsemide, Bumetanide, Metolazone, or Ethacrynic acid each fill a niche.
The key is matching the drug’s pharmacology to your clinical goals, kidney function, side‑effect tolerance, and budget. Use the table and checklist above as a starting point, then discuss with your healthcare provider to fine‑tune the plan.
Frequently Asked Questions
Can I take Furosemide and Hydrochlorothiazide together?
Yes, many doctors combine a loop diuretic with a thiazide to achieve a synergistic “sequential nephron blockade.” This can boost fluid loss while allowing lower doses of each drug, reducing side‑effects. However, close monitoring of electrolytes is essential.
Why does Furosemide sometimes cause ringing in the ears?
High IV doses or rapid infusion can damage the inner ear’s hair cells, leading to ototoxicity. Staying within recommended dosing limits and avoiding rapid bolus injections reduces this risk.
Is Torsemide better for patients with chronic kidney disease?
Torsemide’s longer half‑life and reliable oral absorption make it a good option for CKD patients who can’t tolerate the short peaks of Furosemide. It still works best when GFR is above 15 mL/min.
What should I do if I develop low potassium while on a loop diuretic?
Your doctor may prescribe a potassium‑sparing diuretic (like spironolactone) or a supplement. Foods rich in potassium-bananas, oranges, potatoes-can also help, but don’t self‑adjust doses.
Are there natural alternatives to prescription diuretics?
Some foods (caffeine, dandelion tea) have mild diuretic effects, but they’re nowhere near as potent or controllable as prescription agents. Always talk to a clinician before substituting.




Carla Taylor
October 24, 2025 AT 17:10Furosemide does the job for fast fluid removal but cheaper options like Hydrochlorothiazide work for long‑term blood pressure control
Dawn Bengel
October 24, 2025 AT 18:06Only real doctors trust the classic loop – forget the fancy thiazides 🙄💪
Amanda Vallery
October 24, 2025 AT 19:06Bumetanide is ~40× more potent per mg than furosemide.
Marilyn Pientka
October 24, 2025 AT 20:03The indiscriminate use of furosemide reflects a systemic complacency that undermines personalized medicine. By privileging a one‑size‑fits‑all approach, clinicians ignore pharmacodynamic nuances that could mitigate ototoxic risk. The ethical calculus demands that we prioritize patient‑centred optimisation over pharmaceutical inertia. Moreover, deploying a high‑potency loop without assessing renal reserve contravenes best‑practice guidelines. In short, the reflexive default to Lasix is both clinically lazy and morally indefensible.
Jordan Levine
October 24, 2025 AT 21:01Listen up – if you’re not on furosemide when the heart’s about to explode you’re basically asking for trouble 😡🔥
Michelle Capes
October 24, 2025 AT 22:00I hear the frustration and agree that individualized dosing can prevent many of those avoidable complications. It’s worth taking a moment to review renal function and potassium levels before jumping on a high‑dose loop.
Dahmir Dennis
October 24, 2025 AT 22:58Ah yes, the age‑old mantra: if it works once, keep using it forever. Nothing says "evidence‑based medicine" like ignoring the newer agents just because they’re shiny. I’m sure the patient appreciates the endless bathroom trips for the sake of tradition. Maybe next time we’ll prescribe a placebo and call it progress.
Jacqueline Galvan
October 24, 2025 AT 23:56When deciding between furosemide and its alternatives, the clinician must first evaluate the urgency of diuresis.
If the patient presents with acute pulmonary edema, a rapid‑acting loop such as furosemide or bumetanide is appropriate.
These agents achieve peak natriuresis within an hour, allowing for prompt symptomatic relief.
Conversely, for chronic hypertension management, a thiazide‑type diuretic offers a smoother, longer‑lasting blood pressure reduction.
Hydrochlorothiazide’s half‑life of up to 24 hours makes it suitable for once‑daily dosing.
Torsemide’s improved oral bioavailability can simplify outpatient regimens for patients who struggle with furosemide’s short peaks.
Metolazone remains valuable in low‑GFR states because it retains efficacy where many loops lose potency.
When sulfa allergy limits the use of standard loops, ethacrynic acid provides a non‑sulfonamide alternative, albeit with a higher risk of ototoxicity.
Cost considerations also influence prescribing; generic furosemide and hydrochlorothiazide are among the most affordable options on the market.
However, insurance formularies may favor branded torsemide for its pharmacokinetic advantages, raising out‑of‑pocket expenses.
Electrolyte monitoring is non‑negotiable, especially potassium levels, as hypokalemia predisposes to arrhythmias.
Potassium‑sparing agents such as spironolactone can be co‑prescribed when long‑term loop therapy is unavoidable.
Patient education about weight tracking and fluid intake empowers self‑management and early detection of decompensation.
Finally, always review concomitant NSAID use, which can blunt diuretic efficacy and worsen renal function.
In summary, matching the drug’s pharmacologic profile to the individual’s clinical context yields the safest and most effective outcome.
Tammy Watkins
October 25, 2025 AT 00:55I appreciate the comprehensive overview and would add that the selection of a diuretic should be anchored in evidence‑based protocols rather than habitual prescribing. Moreover, incorporating patient‑reported outcomes can fine‑tune dosing strategies.
junior garcia
October 25, 2025 AT 01:53Great summary! The simple language helps anyone understand the choices.
Dason Avery
October 25, 2025 AT 02:51Philosophically speaking, each diuretic is a tool in the physician’s toolbox, and selecting the right one reflects the art of medicine 😊🌿
Kester Strahan
October 25, 2025 AT 03:50From a pharmaco‑kinetic standpoint, torsemide offers a more predicatable absorption profile; however, one must not overlook the inter‑patient variabillities that can affect bioivailibility.
Doreen Collins
October 25, 2025 AT 04:48Remember, consistency is key – keep an eye on electrolytes and weight trends. If you notice a sudden gain, adjust the dose before things get out of hand. It’s all about staying proactive rather than reactive.
Kathryn Rude
October 25, 2025 AT 05:46Honestly the whole diuretic debate feels like academic elitism overblown it’s just chemistry and patient response – cut the jargon and stick to the facts this is not a philosophy class
Lindy Hadebe
October 25, 2025 AT 06:45Interesting points, though a bit over‑generalized.