Prednisone/Prednisolone Side Effect Risk Calculator
Enter your treatment parameters below to see your personalized risk of common side effects. Based on clinical data from the article content.
When you’re prescribed prednisone or prednisolone, it’s usually because your body is fighting something serious-an autoimmune flare, a bad allergic reaction, or severe inflammation. These drugs work fast. Like, prednisone and prednisolone can turn a debilitating flare-up into something manageable in just a few days. But that speed comes with a cost. Side effects aren’t rare. They’re expected. And knowing what’s coming can make all the difference between feeling overwhelmed and feeling in control.
How These Drugs Work (And Why They Cause Side Effects)
Prednisone and prednisolone are synthetic versions of cortisol, the hormone your adrenal glands naturally make. They’re powerful anti-inflammatories and immunosuppressants. That means they calm down an overactive immune system-great for conditions like lupus, rheumatoid arthritis, or severe asthma. But your body doesn’t know the difference between a real cortisol spike and a drug-induced one. So it reacts the same way: fluids build up, blood sugar rises, bones weaken, and your mood gets tossed around.
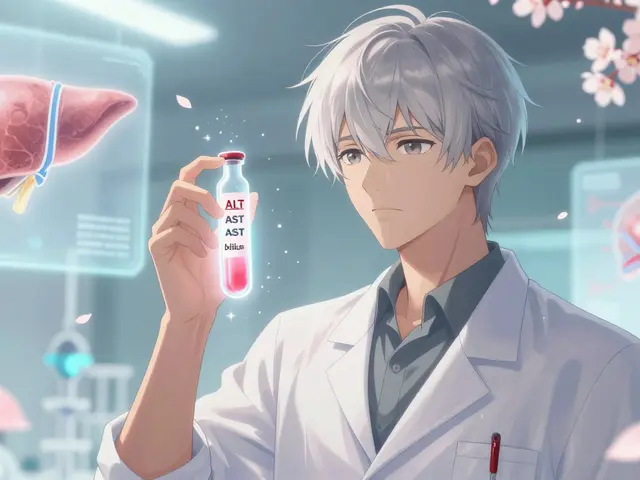
Here’s the key detail most people miss: prednisone isn’t active until your liver turns it into prednisolone. If you have liver damage-say from alcohol, hepatitis, or fatty liver disease-your body can’t convert it well. That’s why doctors sometimes skip prednisone entirely and go straight to prednisolone in those cases. For everyone else, the two are practically interchangeable. A 5mg dose of prednisone equals a 5mg dose of prednisolone in effect. But the side effects? They’re nearly identical.
Short-Term Side Effects: The First Few Weeks
If you’re on these drugs for less than three weeks, you’re likely dealing with the short-term crowd. These aren’t permanent. But they’re real, and they hit hard.
- Insomnia: Over two-thirds of users report trouble sleeping. It’s not just being wired-it’s cortisol disrupting your natural rhythm. Taking your dose before 2 p.m. cuts sleep problems in half.
- Increased appetite and weight gain: You’re not lazy. Your brain is being flooded with signals to eat. Cravings for salty, sugary foods spike. It’s not willpower-it’s biology.
- Mood swings and anxiety: Some people feel euphoric. Others get irritable, paranoid, or even psychotic. One Reddit user described calling 911 at 60mg because he thought spiders were crawling on his walls. That’s not exaggeration-it’s documented.
- Fluid retention and swelling: Your face might puff up (‘moon face’), your ankles swell, and your clothes feel tighter. This isn’t fat. It’s sodium and water stuck in your tissues.
- High blood sugar: Even if you’ve never had diabetes, prednisone can push your glucose into dangerous territory. At doses above 20mg daily, over half of non-diabetics develop steroid-induced hyperglycemia.
These symptoms usually fade within a week or two after stopping the drug. But while you’re on it, they’re exhausting. And they’re why so many people hate these meds-even when they work.
Long-Term Side Effects: The Silent Damage
When you’re on prednisone or prednisolone for more than three months, the game changes. The side effects stop being temporary. They become permanent.
- Osteoporosis and fractures: After two years of use, 63% of long-term users develop bone loss severe enough to be called osteoporosis. Bones become brittle. A simple fall can break a hip or spine. That’s why doctors check bone density after three months on any dose above 5mg daily.
- Cataracts and glaucoma: Your eyes are vulnerable. About 41% of people on long-term steroids eventually need cataract surgery. Glaucoma risk rises too, especially if you’re over 40.
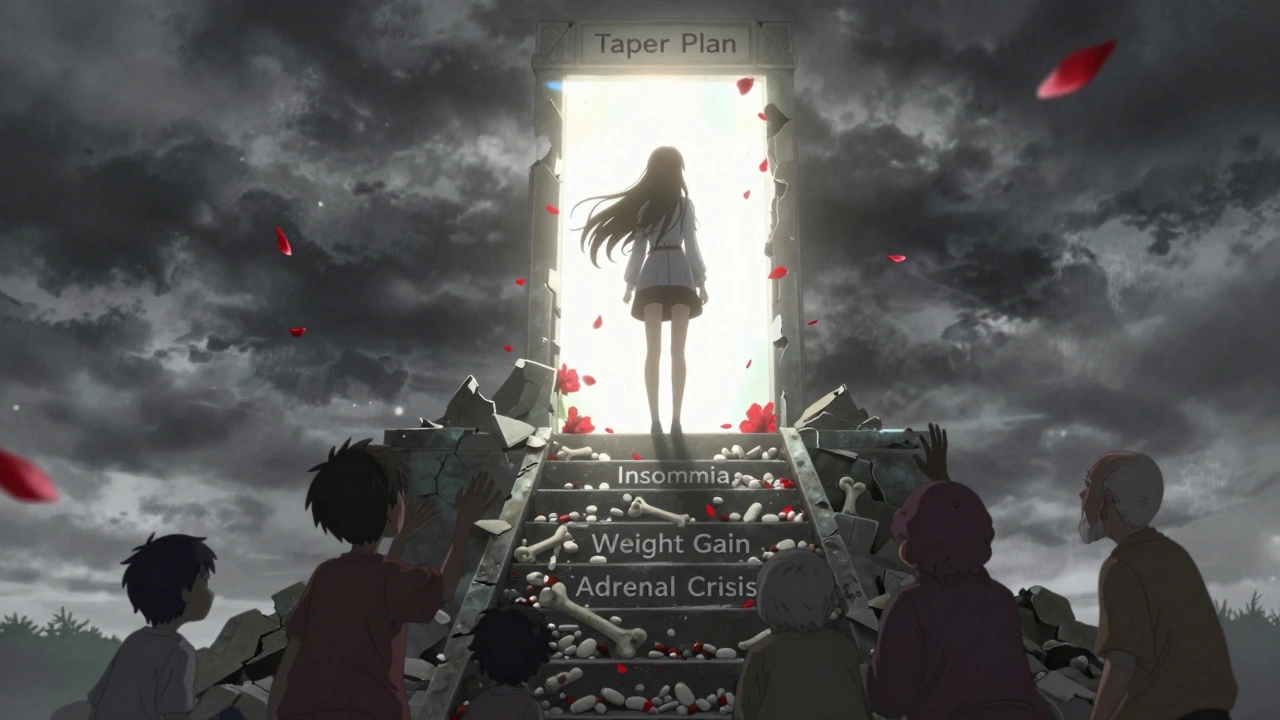
- Adrenal suppression: Your body stops making its own cortisol because it thinks the drug is doing the job. If you stop suddenly, your body can’t catch up. That’s adrenal crisis-low blood pressure, vomiting, confusion, even death. Tapering isn’t optional. It’s life-saving.
- Muscle weakness and wasting: Your legs feel heavy. Climbing stairs becomes a chore. This isn’t aging. It’s steroid-induced myopathy. It improves after stopping, but it can take months.
- Avascular necrosis: Blood flow to your hip or shoulder joint dies. Bone tissue collapses. You might need a joint replacement. This happens in 9% to 40% of people on high doses for more than three months.
- Permanent metabolic changes: Some people never fully recover their insulin sensitivity. Weight stays on. Blood pressure stays high. Diabetes sticks around-even after stopping the drug.
And here’s the hard truth: these risks aren’t rare. They’re predictable. The longer you’re on it, the higher the chance. At 20mg daily for eight weeks, 40% of patients develop at least one serious side effect.

Who Gets Hit Hardest?
Not everyone reacts the same. Kids, older adults, and people with existing health issues face higher risks.
Children: Growth suppression is real. For every 0.2mg per kilogram of body weight per day, kids lose 1.2 centimeters of growth per year. That’s why pediatricians monitor height every three months. Parents often report ‘moon face’ as the most distressing side effect-but the slowed growth is the silent fear.
Older adults: Bone loss and muscle wasting hit harder. Falls are more dangerous. Recovery is slower. Many end up with permanent disability.
People with diabetes or high blood pressure: Prednisone makes both worse. Blood sugar control becomes a daily battle. Blood pressure meds may need adjusting.
People with liver disease: If your liver can’t convert prednisone to prednisolone, you’re getting less of the drug than you think. Your doctor may switch you to prednisolone directly to avoid underdosing.
How to Protect Yourself
These drugs aren’t evil. They’re tools. But like a chainsaw, they’re dangerous if used carelessly. Here’s how to use them safely:
- Take the lowest dose possible. Never assume ‘more is better.’ A 5mg daily dose often works just as well as 10mg.
- Take it early. Taking your dose before 2 p.m. cuts insomnia risk by nearly 60%.
- Protect your bones. Get a bone density scan after three months. Take calcium and vitamin D daily. Walk or lift weights-weight-bearing exercise preserves bone density better than any supplement.
- Watch your sodium. Limit salt to under 2,000mg a day. Eat potassium-rich foods like bananas, spinach, and sweet potatoes to fight fluid retention and low potassium.
- Protect your stomach. If you’re on more than 5mg daily for over four weeks, you should be on a proton pump inhibitor (like omeprazole). It cuts ulcer risk from 8% to under 2%.
- Monitor your blood sugar. Even if you’re not diabetic, check your glucose weekly if you’re on 20mg or more.
- Never stop cold turkey. Tapering takes weeks, sometimes months. Your doctor should give you a schedule. Don’t guess.
What About Alternatives?
There’s no magic bullet that replaces prednisone or prednisolone for acute inflammation. But for long-term management, things are changing.
Biologics like tocilizumab and rituximab are reducing steroid dependence in rheumatoid arthritis by nearly 30%. New drugs called selective glucocorticoid receptor modulators are in trials-they promise the anti-inflammatory power without the weight gain or bone loss. One is showing 60% fewer metabolic side effects in early testing.
But for now? If you’re having a flare, these drugs are still the fastest, most reliable option. The goal isn’t to avoid them-it’s to use them wisely and get off them as soon as possible.
Real Stories, Real Risks
One patient on Drugs.com wrote: ‘I took prednisone for a month for a bad rash. Lost 15 pounds of water weight when I stopped. But my bones feel like they’re crumbling now.’
Another, a mother of a child with Crohn’s disease: ‘My son gained 20 pounds in six weeks. His face looked like a balloon. He cried every night because he didn’t recognize himself. But without it, he couldn’t eat. We had no choice.’
These aren’t outliers. They’re common. And they’re why the American College of Rheumatology says: ‘Use the lowest dose for the shortest time possible.’
That’s the mantra. Not ‘avoid at all costs.’ Not ‘take forever.’ But ‘use smart, get off fast.’
Can prednisone and prednisolone be used interchangeably?
Yes, for most people with healthy livers, 5mg of prednisone equals 5mg of prednisolone in effect. But prednisone must be converted by the liver into prednisolone to work. If you have liver disease, your body may not convert it well-your doctor may switch you to prednisolone directly to ensure you get the full dose.
How long do short-term side effects last after stopping?
Most short-term side effects like insomnia, increased appetite, mood swings, and fluid retention fade within one to two weeks after stopping. Weight gain from water retention drops quickly. Mood changes usually resolve within days. But if you’ve been on it longer than three months, some effects-like bone loss or insulin resistance-may linger.
Is it safe to take prednisone for a month?
A one-month course is common and generally safe for acute conditions like asthma flares or severe allergies. But even a month can cause bone thinning, muscle weakness, and blood sugar spikes. Your doctor should monitor you and give you a taper plan. Never take it longer than prescribed without medical supervision.
What’s the difference between prednisone and prednisolone for children?
Prednisolone is often preferred for kids because it doesn’t require liver conversion. It’s also available in liquid and orally disintegrating tablet forms, making dosing easier. Both cause the same side effects, but prednisolone is more predictable in children, especially those with immature liver function.
Can you get addicted to prednisone?
You don’t get addicted in the way you do to opioids or alcohol. But your body becomes dependent on it. Stopping suddenly can trigger adrenal crisis-a life-threatening drop in cortisol. That’s why tapering is non-negotiable. It’s not addiction. It’s physiology.
Do these drugs cause weight gain forever?
Water weight from fluid retention goes away within weeks after stopping. But fat gain? That’s harder. Steroids increase appetite and change how your body stores fat-especially around the belly and face. Some people lose it with diet and exercise. Others struggle long-term, especially if they developed insulin resistance. It’s not guaranteed, but it’s common enough to be a real concern.
Are there natural alternatives to prednisone?
No natural remedy can match the speed or power of prednisone or prednisolone for acute inflammation. Turmeric, fish oil, or CBD may help with mild chronic inflammation, but they won’t stop a flare of lupus or severe asthma. These drugs are irreplaceable in emergencies. The goal isn’t to replace them with herbs-it’s to use them briefly and then move to safer long-term options.
Final Thought: It’s Not About Fear-It’s About Control
Prednisone and prednisolone aren’t villains. They’re lifesavers when used right. But they’re also weapons that can turn on you if you’re not careful. The key isn’t avoiding them. It’s knowing exactly what you’re signing up for. Track your symptoms. Stick to your taper. Eat right. Move your body. And never, ever stop without your doctor’s plan.
These drugs give you time. Time to heal. Time to find a better long-term solution. Use that time wisely-and don’t let the side effects steal your life after the inflammation is gone.





Albert Essel
December 2, 2025 AT 11:31Prednisone is one of those drugs that feels like a double-edged sword-you get your life back for a few weeks, then spend the next six months trying to undo the damage. I was on it for 10 days for a bad eczema flare, and I swear I gained 8 pounds of water weight overnight. My face looked like a balloon. But honestly? Worth it. Just don’t lie to yourself about the toll it takes.
Also, taking it before 2 p.m.? Non-negotiable. I tried taking it at night once. Slept for 90 minutes total. Didn’t even know my body could feel that wired.
Charles Moore
December 3, 2025 AT 22:41This is one of the clearest, most compassionate breakdowns of steroid side effects I’ve ever read. Seriously, thank you for writing this. Too many docs just hand out prescriptions like candy and never explain what’s coming. I’ve seen friends go from vibrant to hollow-eyed in a month on prednisone. The emotional toll is often worse than the physical. You’re right-it’s not about fear, it’s about control. And control means knowing the clock is ticking.
Also, the liver conversion point? Huge. My uncle had cirrhosis and was on prednisone for months before anyone realized he wasn’t converting it. He was basically getting half-doses. That’s medical negligence waiting to happen.
Gavin Boyne
December 4, 2025 AT 22:10Oh wow, a medical article that doesn’t sound like it was written by a pharmaceutical rep pretending to be a caring nurse. What a novelty.
Let me guess-the next paragraph says ‘consult your doctor’ and then quietly slips in a link to the brand-name version of prednisolone. But hey, at least you didn’t say ‘just eat more kale and meditate.’ That’s progress, I guess.
Also, ‘moon face’? That’s the most accurate term ever coined for steroid side effects. It’s not puffiness. It’s your face turning into a harvest moon. I’ve seen grown men cry over it. And no, you can’t ‘just work it off.’ Your body isn’t a gym app.
Rashi Taliyan
December 5, 2025 AT 11:21I’m from India and my sister was on prednisone for lupus for 18 months. She lost her period. Her hair fell out in clumps. She couldn’t climb stairs without stopping. And the worst part? She couldn’t look in the mirror without crying. We had to hide the full-length mirror in the bathroom. But she’s alive. And that’s the trade-off. No one talks about how it steals your identity. You’re not just sick-you’re unrecognizable. I wish I’d known this before she started.
Also, please, doctors-don’t just say ‘it’s temporary.’ It’s not. Not for her. Not for so many of us.
Kara Bysterbusch
December 6, 2025 AT 00:54It is with profound appreciation that I acknowledge the meticulous articulation of the pharmacological and physiological implications of corticosteroid therapy as delineated in this exposition. The precision with which the dichotomy between short-term palliation and long-term iatrogenic morbidity is elucidated is both academically rigorous and clinically indispensable.
Furthermore, the emphasis upon hepatic biotransformation as a determinant of therapeutic efficacy constitutes a critical, yet frequently overlooked, nuance in clinical decision-making. The correlation between prolonged administration and the development of avascular necrosis, osteoporosis, and metabolic syndrome is not merely statistical-it is existential for the patient population.
One must, however, remain vigilant against the romanticization of ‘natural alternatives,’ as such narratives often stem from a dangerous conflation of anecdote with evidence. The efficacy of turmeric in suppressing acute systemic inflammation is negligible compared to the potency of glucocorticoid receptor modulation. This is not to diminish integrative medicine, but to affirm the non-negotiable role of evidence-based intervention in acute, life-altering conditions.
Rashmin Patel
December 6, 2025 AT 17:02OMG I was on this for 3 months after my kidney transplant and I thought I was going crazy 😭 I gained 30 lbs in 8 weeks, my face looked like a cartoon, I was crying for no reason, and my mom had to stop me from buying 7 pizzas in one day 😂 I didn’t even like pizza before!!
And then when I stopped?? My body just… gave up. I was so weak I couldn’t lift my own coffee mug. Took 4 months to feel like myself again. My bones are still weak. I’m 28. I shouldn’t be getting osteoporosis warnings.
But here’s the thing-I’d do it again. My transplanted kidney would’ve failed without it. So yes, it’s hell. But sometimes hell is the only way out.
PS: Take calcium. Like, a LOT. And walk. Even if it’s just around the living room. I did it. My bones are still here. 💪
Cindy Lopez
December 8, 2025 AT 11:03Interesting. I’ve been on this for six months. Haven’t gained weight. Slept fine. No mood swings. So either you’re exaggerating, or I’m just lucky. Maybe you’re just weak.
Also, why are you all acting like this is a horror movie? It’s medicine. Take it. Stop whining.
James Kerr
December 10, 2025 AT 03:04Man, I read this and just nodded the whole time. I was on 40mg for 3 weeks for a bad asthma attack. Felt like a superhero for the first week. Then… boom. I couldn’t open a jar. My legs felt like wet noodles. And I ate like a bear in hibernation.
But the sleep thing? Yeah. I was up at 3 a.m. every night scrolling TikTok like a zombie. Took me a week to sleep normal after I stopped.
Just… take it early. And don’t be ashamed if you need help. This stuff is rough. You’re not weak. It’s just science being a jerk.
shalini vaishnav
December 11, 2025 AT 05:30This is Western medical arrogance at its finest. In Ayurveda, we have herbs like Ashwagandha and Guduchi that modulate immune response without destroying the body’s natural balance. You people are so addicted to synthetic chemicals you forget the body has its own intelligence.
And you say ‘no natural alternative’? That’s ignorance. We’ve been treating inflammation for 5,000 years without prednisone. Your ‘lifesaver’ is a crutch for lazy medicine. You treat symptoms, not root causes. That’s why you have so many side effects.
Stop glorifying pharmaceutical dependency. It’s not science. It’s colonialism in pill form.
vinoth kumar
December 12, 2025 AT 16:15My dad took this for rheumatoid arthritis for 2 years. He got cataracts. Lost 30% of his bone density. But he could walk again. He could hold my baby. He could hug us without screaming in pain.
So yeah, it wrecked him. But it gave him back his life. That’s not a trade-off. That’s a miracle.
Just please, doctors-don’t forget to check on the people after they stop. We’re not done when the prescription ends. We’re just starting to heal.
Katherine Gianelli
December 14, 2025 AT 04:36I wish I’d read this before I started. I took it for a month for a bad case of allergic bronchitis. Thought I’d be fine. I wasn’t.
My skin started peeling like a sunburn. I couldn’t sleep. I gained 12 pounds of water weight. My blood sugar spiked so high I had to start checking it daily.
And when I stopped? I didn’t taper. Just quit. Felt fine at first. Then two days later, I collapsed in the grocery store. Paramedics said I was in adrenal crisis.
Don’t be like me. Taper. Even if you feel good. Even if your doctor says ‘it’s fine.’ Your body remembers.
And if you’re a parent? Watch your kid’s growth chart like a hawk. I didn’t. My daughter lost 3 inches of potential height. I didn’t know it until it was too late.
Joykrishna Banerjee
December 14, 2025 AT 06:10Let’s be real-this is just Big Pharma’s way of keeping people dependent on chronic medication. You know how many people get stuck on prednisone because they’re too scared to taper? Because their doctors don’t have a plan? Because they’re too lazy to find alternatives?
Biologics? Sure. But they cost $50k a year. So instead, we give people a cheap, toxic band-aid and call it ‘care.’
And you say ‘use smart, get off fast’? That’s not a plan. That’s a slogan. Where’s the infrastructure? Where’s the support? Where’s the follow-up? Nowhere. That’s why people suffer.
It’s not the drug. It’s the system.
Myson Jones
December 15, 2025 AT 06:33Thank you for writing this with such clarity. I’m a nurse, and I’ve seen too many patients come in terrified because they didn’t know what to expect. This is the kind of info we should be handing out with the script.
One thing I’d add: the weight gain isn’t just from appetite. Steroids change your fat distribution. Belly fat sticks. Even if you lose the water, the visceral fat hangs on. It’s not laziness. It’s biology.
And for the love of God-don’t let patients skip calcium. I’ve seen too many hip fractures in 45-year-olds because they thought ‘I’m too young for osteoporosis.’ You’re not.
parth pandya
December 15, 2025 AT 07:00Hey i read this and its really good but i think you miss one thing-some people get acne so bad it looks like they have a whole face of cysts. Like full on teenage breakout but at 52. I know a guy who stopped prednisone and his skin was still wrecked for 8 months. No one warned him. Just said ‘it’ll go away.’
Also, if you’re on it long term, get your eyes checked every 6 months. Cataracts don’t wait.
sagar bhute
December 16, 2025 AT 17:02Everyone’s acting like this is some tragic tragedy. You’re on a drug that suppresses your immune system. Of course you’re going to gain weight, get diabetes, and lose bone density. That’s what it’s supposed to do. You want a magic pill? There isn’t one.
If you can’t handle the side effects, don’t take it. Simple. Stop whining. You’re alive because of this. Act like it.
Albert Essel
December 17, 2025 AT 10:19Just read the comment from the nurse. That’s the real story. I didn’t know about the visceral fat thing. My jeans still don’t fit, even though I’ve lost 15 pounds since stopping. It’s not fat. It’s like my body decided to keep the steroid version of me.
And the skin thing? Yeah. I got acne so bad I started wearing hoodies in July. No one talks about that. Just the moon face.
Thanks for the reminder. I’m getting my eyes checked next week.