Warfarin Vitamin K Tracker
Daily Vitamin K Tracker
Track your vitamin K intake to maintain stable INR levels. Consistency is key with warfarin.
Your Current Vitamin K Intake
Daily recommended intake: 90 mcg (women) / 120 mcg (men)
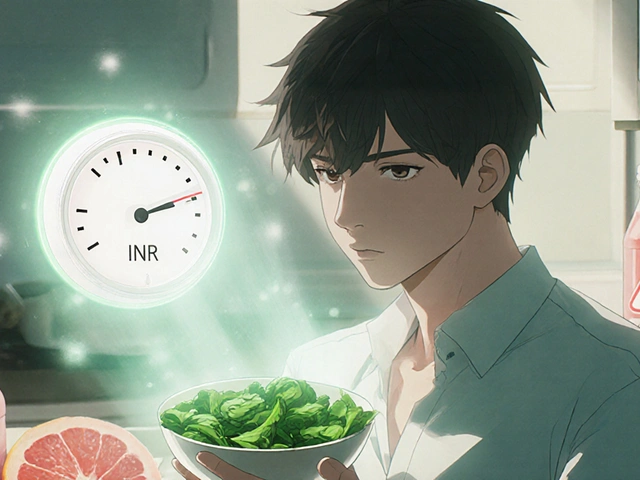
When you're on warfarin, what you eat isn't just about nutrition-it can mean the difference between a blood clot and a dangerous bleed. Warfarin works by blocking vitamin K, a nutrient your body needs to make blood clot. But if your vitamin K intake jumps around, your blood can become too thin or not thin enough. That’s why consistency, not elimination, is the golden rule.
How Warfarin Actually Works
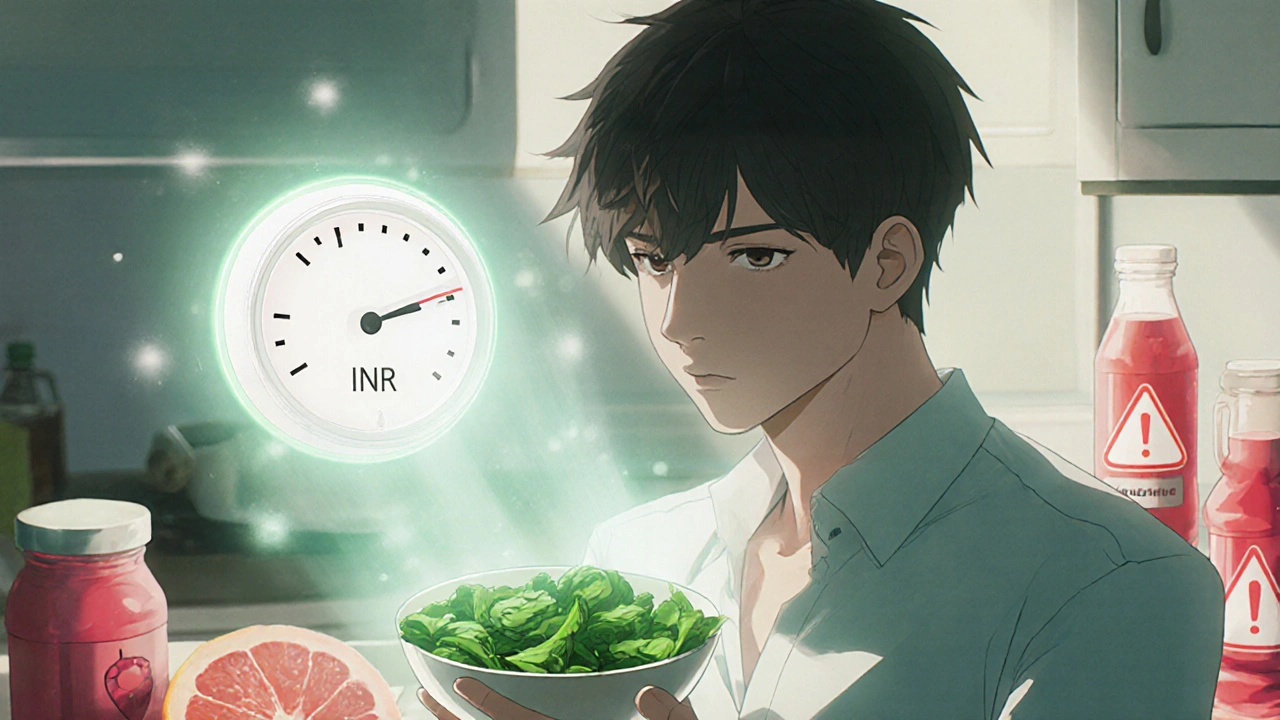
Warfarin doesn’t thin your blood like water. It slows down the production of clotting factors that depend on vitamin K. Think of vitamin K as a switch that turns on these factors. Warfarin flips that switch off. But if you suddenly eat a lot of vitamin K-say, a big plate of kale-the switch gets flipped back on, and your blood starts clotting again. That’s why your INR (a measure of how long it takes your blood to clot) can swing wildly with inconsistent eating.
Your target INR is usually between 2.0 and 3.0. If it drops below 2.0, clots can form. If it goes above 3.0, you risk bleeding inside your brain, gut, or joints. A single serving of cooked spinach-about 889 micrograms of vitamin K-can shift your INR by 0.5 to 1.0 points in just a few days. That’s enough to land you in the ER.
The Vitamin K Food List: What to Eat (and What to Avoid)
You don’t need to give up greens. You need to eat them the same way every day.
- Very High Vitamin K (>500 mcg per 100g): Kale (817 mcg), collard greens (623 mcg), parsley (616 mcg), seaweed (599 mcg), spinach (483 mcg), Swiss chard (450 mcg), turnip greens (421 mcg). One cup of cooked spinach has more vitamin K than your entire daily need.
- High Vitamin K (100-500 mcg per 100g): Broccoli (102 mcg raw), Brussels sprouts (177 mcg), cabbage (60 mcg cooked), lettuce (30 mcg raw), green tea (106 mcg per cup).
- Medium Vitamin K (25-100 mcg per 100g): Asparagus (70 mcg cooked), avocado (21 mcg), cucumber (16 mcg), carrots (13 mcg), eggs (12 mcg).
Here’s the catch: if you normally eat a small salad with spinach every day, keep doing it. If you never eat greens, don’t suddenly start eating two cups of kale every morning. That spike will crash your INR. Consistency beats perfection.
Top 5 Foods and Drinks That Can Mess With Warfarin
It’s not just vitamin K. Other common items can interfere with how your body breaks down warfarin.
- Cranberry juice: Even a single 8-ounce glass can raise your INR by 1 to 2 points. It blocks the enzyme (CYP2C9) that clears warfarin from your body. One Reddit user saw his INR jump from 2.4 to 4.1 after daily cranberry juice. That’s a bleeding risk.
- Grapefruit juice: It slows down another enzyme (CYP3A4), making warfarin stick around longer. Clinical reports show a 30% increase in bleeding risk. Don’t drink it at all.
- Alcohol: More than two drinks a day lowers warfarin’s effectiveness by 15-20%. Heavy drinking can also damage your liver, which makes warfarin harder to process. Stick to one drink occasionally, and never binge.
- Fish oil supplements: Omega-3s thin your blood on their own. Combined with warfarin, bleeding risk goes up by 25%. Talk to your doctor before taking any fish oil.
- Garlic supplements: Raw garlic in food is fine. But garlic pills? They can raise your INR by 0.8 to 1.2 units. Same goes for ginkgo biloba-case reports show it increases bleeding risk by 40%.
What About Other Supplements and Herbal Products?
Many people think “natural” means safe. That’s not true with warfarin.
- St. John’s Wort: Speeds up warfarin metabolism. Lowers INR. Can cause clots.
- Coenzyme Q10: Has vitamin K-like activity. May reduce warfarin’s effect.
- Chamomile, green tea (in large amounts), and ginger: Can increase bleeding risk.
- Vitamin E supplements (over 400 IU/day): May thin blood further.
Always tell your anticoagulation clinic about every supplement, herb, or over-the-counter pill-even if you think it’s harmless. A 2023 study found that 61% of warfarin patients took at least one supplement without telling their doctor.
How to Eat Consistently (Without Going Crazy)
Here’s what works for people who’ve stayed stable for years:
- Pick your greens and stick to them. If you like spinach, have one cup cooked every day. If you prefer lettuce, have two cups raw every day. Don’t switch.
- Use a food tracking app. MyFitnessPal lets you log vitamin K intake. People who track their food have 22% fewer out-of-range INR tests.
- Plan meals ahead. If you know you’ll have a big dinner with broccoli and kale, don’t eat more greens at lunch.
- Don’t skip meals. Skipping meals changes how your body absorbs warfarin.
- Keep a food journal. The American Thrombosis Association found that 76% of people who kept a daily food log stayed in their target INR range 70% of the time. Those who didn’t track? Only 48%.
One patient on PatientsLikeMe said: “I eat exactly one cup of spinach salad every day, no more, no less. I’ve had the same INR for 18 months. Consistency is everything.”
When to Call Your Doctor Immediately
Warfarin side effects can sneak up. Don’t wait for a lab test. Watch for these signs:
- Bleeding that won’t stop after 5 minutes (even from a small cut)
- Black, tarry, or bloody stools
- Unexplained bruising, especially large purple patches
- Severe headache, dizziness, or vision changes (could be brain bleed)
- Red or pink urine
- Unusual joint pain or swelling (could be internal bleeding)
CDC data shows that 18% of warfarin-related ER visits are due to bleeding that lasts longer than 5 minutes. If you notice any of these, call your doctor or go to urgent care. Don’t wait for your next INR check.
What About Newer Blood Thinners?
Drugs like apixaban (Eliquis) and rivaroxaban (Xarelto) don’t need diet changes or regular blood tests. That’s why they’re becoming more popular. But warfarin is still the best choice for some people:
- People with mechanical heart valves (85% still use warfarin)
- Those with severe kidney disease (DOACs aren’t cleared well)
- Patients who can’t afford the newer drugs (warfarin costs about $5 a month)
So even though DOACs are easier, warfarin isn’t going away. The key is mastering your diet.
What’s New in Warfarin Management
In 2024, the FDA approved a new tool called WarfarinDoseIQ-a dosing algorithm that adjusts your warfarin dose based on your daily vitamin K intake. It’s being tested in clinics now.
Companies like Nutrisystem have launched meal kits with exactly 25-30 mcg of vitamin K per meal, designed for warfarin users. And smart plates that scan food for vitamin K content are in early trials.
But here’s the reality: a 2023 study found that only 58% of patients at safety-net hospitals got proper dietary counseling. If you’re not getting clear advice, ask for an anticoagulation clinic referral. Hospitals with dedicated teams have 15-20% better INR control.
Final Advice: Don’t Fear Food-Control It
Warfarin isn’t a prison sentence. It’s a partnership between you and your diet. You don’t have to eat bland food. You don’t have to give up vegetables. You just need to make your intake predictable.
Start today: write down what you ate yesterday. Look up the vitamin K content. Do it again tomorrow. In two weeks, you’ll see a pattern. In a month, your INR will stabilize. And you’ll be safer than most people on warfarin.
Can I eat spinach if I’m on warfarin?
Yes, you can eat spinach-but only if you eat the same amount every day. One cup of cooked spinach has nearly 900 mcg of vitamin K. If you normally eat one cup daily, keep doing it. If you’ve never eaten it before, don’t start suddenly. Consistency matters more than avoiding it.
Does cranberry juice really affect warfarin?
Yes. Cranberry juice can raise your INR by 1 to 2 points by blocking how your body breaks down warfarin. Even small amounts, like one glass a day, can be dangerous. Avoid it completely. The same goes for cranberry supplements.
Is it safe to drink alcohol while on warfarin?
One drink occasionally is usually okay. But more than two drinks a day lowers warfarin’s effect and increases bleeding risk. Heavy drinking also harms your liver, which processes warfarin. Stick to no more than one drink per day, and skip alcohol at least two days a week.
Should I stop eating green vegetables?
No. Green vegetables are healthy. The goal isn’t to avoid them-it’s to eat the same amount every day. Sudden changes in vitamin K intake are what cause dangerous INR swings. Pick a serving size you can stick with and keep it steady.
How often should I get my INR checked?
When you first start warfarin, you’ll need checks every few days to weeks. Once your dose and diet are stable, checks can go to every 4-6 weeks. But if you change your diet, start a new supplement, get sick, or start antibiotics, you’ll need a check within 3-5 days.
Can I take aspirin or ibuprofen while on warfarin?
No. Aspirin and ibuprofen increase bleeding risk when combined with warfarin. Use acetaminophen (Tylenol) for pain instead. Always check with your doctor before taking any pain reliever, even over-the-counter ones.
What should I do if I miss a dose of warfarin?
Don’t double up. Call your anticoagulation clinic right away. They’ll tell you whether to take the missed dose or skip it, based on your INR and schedule. Never guess-it can lead to clotting or bleeding.
Next Steps: Take Control of Your Diet
Here’s what to do today:
- Check your last INR result. Is it in range?
- Write down everything you ate yesterday.
- Look up the vitamin K content of your top three foods.
- Decide on one consistent serving of greens or vegetables to eat daily.
- Call your doctor’s office and ask if you’re enrolled in an anticoagulation clinic.
Warfarin works best when you’re in charge of your diet-not the other way around. You don’t need to be perfect. You just need to be predictable.





Joseph Peel
November 17, 2025 AT 07:07Consistency is the only thing that matters with warfarin. I’ve been on it for seven years. I eat one cup of cooked spinach every single day, no exceptions. My INR hovers at 2.7. No surprises. No ER visits. No guesswork. If you can’t commit to the same portion size daily, you shouldn’t be on warfarin.
Kelsey Robertson
November 18, 2025 AT 06:43Let’s be real-this whole ‘consistency’ thing is a corporate myth designed to keep you dependent on the system. Why not just switch to a DOAC? They don’t care what you eat. Why are we still torturing people with kale math? The FDA approved new anticoagulants for a reason. This article feels like a pharmaceutical pamphlet disguised as medical advice.
Joseph Townsend
November 20, 2025 AT 02:25Oh my god. I just read this and I’m shaking. I had a kale smoothie last Tuesday. I thought I was being healthy. Now I’m convinced I almost bled out in my sleep. I’ve been taking garlic supplements for my cholesterol. I just Googled ‘garlic + warfarin + death’ and there are 12,000 results. I’m calling my doctor at 3 a.m. I might need a priest. I might need a lawyer. I might need a new identity.
Bill Machi
November 20, 2025 AT 07:59This is a disgrace. America is falling apart because people don’t follow basic medical instructions. You can’t just eat whatever you want and expect your body to compensate. This isn’t a buffet. This is life-or-death pharmacology. The fact that people need a 2,000-word guide to eat spinach responsibly is a national embarrassment. We need mandatory education. We need fines. We need consequences.
Elia DOnald Maluleke
November 20, 2025 AT 20:11In the grand tapestry of human health, warfarin stands as a testament to the fragile equilibrium between nature and science. To manipulate coagulation pathways through dietary restraint is not merely medical-it is philosophical. The spinach, the cranberry, the garlic-they are not enemies. They are mirrors. They reflect our discipline, or our chaos. To eat consistently is to honor the rhythm of the body. To fluctuate is to dance with entropy.
satya pradeep
November 22, 2025 AT 10:22Bro this is gold. I’m on warfarin since 2020 and I eat 1 cup spinach every day like clockwork. My doc says I’m the model patient. But here’s the thing-most people dont even know what vitamin K is. I told my cousin who just got prescribed warfarin and he asked if he can eat pizza. Like bro, pizza has no vitamin K, but the cheese and pepperoni? Still check with doc. Just be consistent. Not perfect. Consistent.
Prem Hungry
November 23, 2025 AT 05:58Dear friend, your dedication to consistency is admirable. I have witnessed many patients struggle with this very issue. The human mind seeks variety, yet the body thrives on rhythm. I urge you to maintain your daily greens, track your intake, and never underestimate the power of a simple journal. You are not alone. Many walk this path with you. Stay steady. Stay safe.
Leslie Douglas-Churchwell
November 25, 2025 AT 03:02Okay but have you considered that the entire vitamin K narrative is a distraction? 🤔 Big Pharma wants you to think it’s about spinach, but it’s really about control. Why do you need weekly INR tests? Why not just switch to the $15,000/year DOACs? 🤨 The real agenda: keep you dependent on the system. Also, I heard the FDA’s new ‘WarfarinDoseIQ’ was developed by a company owned by a former Pfizer exec. 🕵️♀️ #WakeUp
shubham seth
November 25, 2025 AT 22:26This whole post is a glorified diet plan with a side of fearmongering. You say ‘don’t eat cranberry juice’ but ignore that 90% of the studies linking it to INR spikes were done on rats. And what about the 2021 meta-analysis showing no significant interaction? You cherry-pick case reports like they’re gospel. Meanwhile, the real killer? Poor adherence to dosing schedules. But nope-let’s blame the kale.
Kathryn Ware
November 26, 2025 AT 03:27I just want to say how incredibly helpful this is. I’ve been on warfarin for five years and I used to panic every time I ate something green. Now I use MyFitnessPal to log vitamin K and it’s been a game-changer. I even made a spreadsheet for my mom so she can help me track. I’ve had 18 months of rock-solid INRs. If you’re reading this and you’re scared-you’re not alone. But you can do this. It’s not about perfection. It’s about showing up, day after day. You’ve got this. 💪❤️
kora ortiz
November 27, 2025 AT 00:23Joseph Peel
November 29, 2025 AT 00:17^This. Exactly this. I’ve been doing this for seven years. One cup. Every day. No drama. No panic. No ‘what if I eat more?’ Just consistency. The system works if you don’t break it. Stop overthinking. Start eating.