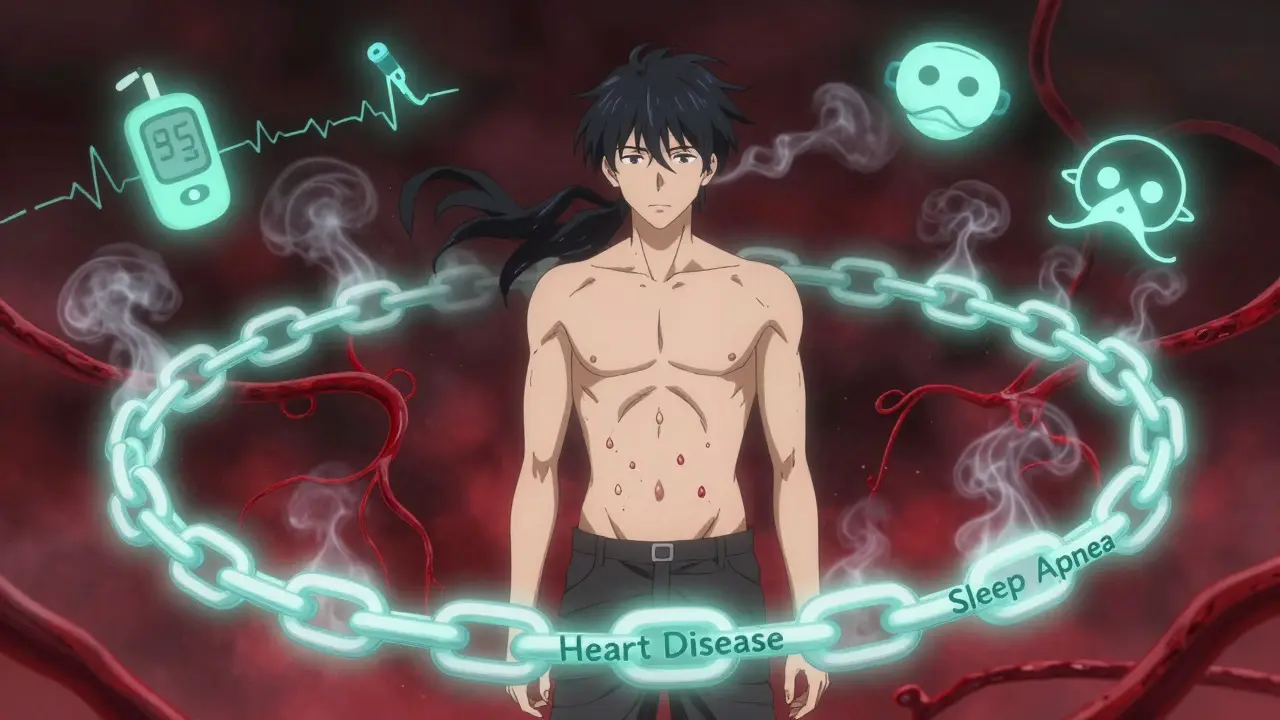
When you hear the word obesity, most people think of weight alone. But for millions of people, obesity isn’t just about clothing sizes or scale numbers. It’s the root of a dangerous chain reaction that affects the heart, the brain, the lungs, and the entire metabolic system. Three conditions - type 2 diabetes, heart disease, and sleep apnea - don’t just happen alongside obesity. They are directly fueled by it. And they feed each other in ways that make things worse over time.
The Triad No One Talks About
Obesity doesn’t sit quietly in the background. It’s an active player in three major health crises. The connection isn’t coincidence. It’s biology. When body fat builds up, especially around the belly, it doesn’t just take up space. It starts releasing chemicals that turn the body against itself. Fat tissue becomes inflamed. Hormones get scrambled. Blood pressure creeps up. Blood sugar spirals out of control. And the airway? It gets squeezed shut during sleep. This isn’t theory. It’s data. A 2018 study called SLEEP-AHEAD found that 86% of obese people with type 2 diabetes also had sleep apnea. And 14% of them already had heart disease. That’s not random. It’s a pattern. Obesity is the spark. Diabetes, heart disease, and sleep apnea are the flames.How Obesity Triggers Diabetes
Your body uses insulin to move sugar from your blood into your cells for energy. When you carry excess fat - especially visceral fat around your organs - your fat cells start pumping out inflammatory signals. These signals make your muscles and liver resistant to insulin. That means your pancreas has to work harder, pumping out more insulin just to keep blood sugar in check. Eventually, it burns out. That’s when type 2 diabetes kicks in. The numbers don’t lie. Obese individuals have 30-50% higher levels of inflammation markers like C-reactive protein and interleukin-6 than people at a healthy weight. That inflammation is the engine behind insulin resistance. And once diabetes sets in, it makes everything else worse. High blood sugar damages blood vessels. It makes the heart work harder. It increases the risk of nerve damage, which can weaken the muscles that keep your airway open during sleep.Sleep Apnea: The Silent Aggravator
Sleep apnea isn’t just loud snoring. It’s when your airway collapses during sleep, stopping breathing for 10 seconds or longer - sometimes hundreds of times a night. In obese people, fat builds up in the neck, tongue, and throat. That’s not just extra tissue. It’s a physical blockage. Every extra pound of BMI increases your risk of sleep apnea by 14%, according to the Wisconsin Sleep Cohort Study. But here’s the twist: sleep apnea doesn’t just happen because of weight. It makes weight harder to lose. Every time your airway closes, your brain jolts you awake to breathe. These mini-awakenings prevent deep, restorative sleep. Without good sleep, your body produces more ghrelin (the hunger hormone) and less leptin (the fullness hormone). You crave carbs. You feel too tired to move. Your metabolism slows. It’s a loop: obesity causes sleep apnea, and sleep apnea makes obesity worse. Worse still, the repeated drops in oxygen during apnea episodes trigger surges in blood pressure and stress hormones. That’s why people with severe sleep apnea (more than 30 breathing pauses per hour) have a 60% higher risk of developing type 2 diabetes - even after accounting for their weight.
Heart Disease: The Deadly Endgame
Now add heart disease into the mix. Obesity alone increases your risk of high blood pressure, abnormal cholesterol, and enlarged heart muscle. Sleep apnea adds nightly spikes in blood pressure - sometimes 15-25 mmHg higher than normal. Diabetes speeds up the clogging of arteries. Together, they create a perfect storm. People with all three conditions face a 3.2-fold higher risk of heart attack than those with obesity alone and no other comorbidities. Heart failure risk jumps to 3.7 times higher when you have obesity, sleep apnea, and diabetes together. And the numbers don’t stop there. Severe sleep apnea increases stroke risk by 68% and coronary artery disease by 58%, even when you control for age, smoking, and other traditional risk factors. A 2022 study in Circulation found that untreated sleep apnea in obese diabetic patients increased cardiovascular death risk by 86%. That’s not a small number. That’s a warning sign.Why Doctors Miss This
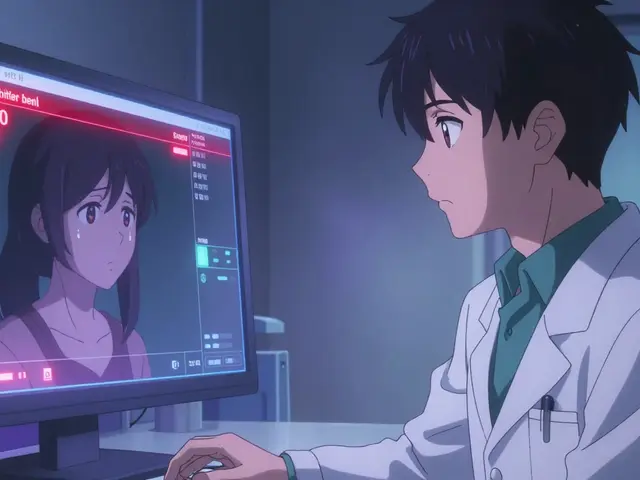
Here’s the frustrating part: most doctors treat each condition separately. You see your endocrinologist for diabetes. Your cardiologist for blood pressure. Your primary care doctor for weight. But who’s asking about your sleep? A 2022 survey from the Obesity Action Coalition found that 74% of obese people with diabetes and sleep apnea reported excessive daytime sleepiness - but only 17.8% of them had ever been screened for sleep apnea. Many patients say their doctors focused only on their blood sugar or weight loss, never connecting the dots to sleep. The American Diabetes Association now recommends screening all obese patients with diabetes for sleep apnea. The tool? The STOP-Bang questionnaire. It asks about snoring, tiredness, observed apneas, high blood pressure, BMI, age, neck size, and gender. A score of 3 or higher means you need a sleep study.
Breaking the Cycle
The good news? This cycle can be broken. And the most powerful tool isn’t a drug - it’s weight loss. Losing just 10-15% of your body weight reduces sleep apnea severity by about half. In one study, obese patients with diabetes who lost weight and used CPAP for six months dropped their HbA1c (a measure of blood sugar control) by 0.8% - a clinically meaningful change. They also lost an average of 3.2 kg without changing their diet or exercise beyond the initial program. CPAP therapy - a machine that blows gentle air through a mask to keep your airway open - is the gold standard for sleep apnea. But it only works if you use it. Only 45% of people stick with CPAP after a year. Common reasons? Mask discomfort, claustrophobia, or just feeling like the pressure is too strong. New options are emerging. The FDA-approved Inspire device, a small implant that stimulates the nerve controlling the tongue, helps patients who can’t tolerate CPAP. And new diabetes medications like semaglutide (Ozempic, Wegovy) don’t just help with weight loss - they reduce fat around the airway, improving sleep apnea even before major weight loss occurs.What You Can Do Right Now
If you have obesity and one of these conditions, don’t wait. Ask for screening for the others.- If you have type 2 diabetes, ask your doctor: “Could I have sleep apnea?”
- If you’re overweight and feel exhausted during the day, get tested for sleep apnea - even if you don’t snore loudly.
- If you have sleep apnea and high blood pressure, get your blood sugar checked.
- If you’re trying to lose weight, know that even modest loss (5-10%) can improve all three conditions.
The Bigger Picture
The economic cost of this triad is staggering. People with obesity, diabetes, and sleep apnea pay $12,300 more per year in healthcare costs than those with obesity alone. Most of that goes to heart-related hospitalizations and emergency visits. But the human cost is worse. People miss work. They get into car accidents from drowsiness. They lose energy to play with their kids. They feel trapped in a cycle they don’t understand. The solution isn’t just more pills or surgeries. It’s awareness. It’s connection. It’s seeing obesity not as a standalone issue, but as the starting point of a chain reaction - one that can be interrupted. Your weight matters. But what matters more is what that weight is doing to your body behind the scenes. Diabetes, heart disease, and sleep apnea aren’t separate problems. They’re symptoms of the same root cause. And fixing that root cause - even slowly - can change everything.Is obesity the direct cause of sleep apnea?
Obesity is the leading cause of obstructive sleep apnea, but not the only one. About 70-80% of OSA cases occur in people with a BMI over 30. Fat deposits in the neck and throat physically narrow the airway. Each 1-unit increase in BMI raises OSA risk by 14%. However, 20-25% of people with sleep apnea are not obese - these cases often involve jaw structure, genetics, or neuromuscular issues.
Can losing weight cure sleep apnea?
Yes, for many people. Losing 10-15% of body weight can reduce sleep apnea severity by 50% or more. In one study, people who lost 10% of their weight saw their apnea-hypopnea index (AHI) drop from 30 to 15 events per hour - from severe to mild. Bariatric surgery leads to remission in 78% of cases. But weight loss alone doesn’t guarantee complete resolution - some structural changes in the airway may remain.
Does treating sleep apnea help with diabetes?
Absolutely. Treating sleep apnea with CPAP improves insulin sensitivity. A 2021 study showed that obese diabetic patients using CPAP for 6 months lowered their HbA1c by an average of 0.8%, which is as effective as adding a second diabetes medication. Better sleep reduces stress hormones, lowers inflammation, and helps your body respond better to insulin.
Why don’t more doctors screen for sleep apnea in obese patients?
Many doctors still view sleep apnea as a snoring issue, not a metabolic disease. There’s also a lack of time, training, and reimbursement for sleep screenings. Only 17.8% of obese patients with diabetes get screened, according to national data. But guidelines from the American Diabetes Association and American Heart Association now strongly recommend routine screening - especially for those with high blood pressure, fatigue, or uncontrolled blood sugar.
Are there alternatives to CPAP for sleep apnea?
Yes. For those who can’t tolerate CPAP, options include oral appliances (custom mouthpieces that hold the jaw forward), positional therapy (sleeping on your side), and newer devices like the Inspire hypoglossal nerve stimulator - an implant that activates throat muscles during sleep. Weight loss remains the most effective long-term solution. In some cases, surgery to remove excess tissue in the throat may be considered, though it carries risks.
Can new diabetes medications like Ozempic help with sleep apnea?
Yes. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) not only cause significant weight loss (up to 15% of body weight) but also reduce fat deposits around the upper airway, even before major weight loss occurs. The 2024 LEADER-OSA trial showed that these drugs improved sleep apnea severity independently of weight loss, likely by reducing inflammation and fat in the throat. This makes them a powerful tool for patients with all three conditions.





Samuel Mendoza
January 21, 2026 AT 08:21Obesity doesn't cause anything. It's just a symptom of laziness and poor willpower. People choose to eat junk and sit on their asses. Stop blaming biology.
MARILYN ONEILL
January 22, 2026 AT 04:17OMG I knew it. My cousin had all three and now she's dead at 42. They never told her about sleep apnea. This is a scam by Big Pharma and doctors to sell CPAP machines. I saw it on TikTok.
Yuri Hyuga
January 23, 2026 AT 18:16This is one of the most important posts I've read all year 🙏
Obesity isn't a moral failure-it's a metabolic emergency. And the fact that we treat diabetes, heart disease, and sleep apnea like separate problems is like treating a house fire by only putting out the kitchen flames while the attic burns.
If you're carrying extra weight and feel tired all day? Get screened. Don't wait. Your heart, your brain, your future kids-they're all counting on you to act now. You're not broken. You're just under-supported.
Small steps matter. One less soda. One walk after dinner. Asking your doctor: 'Could this be sleep apnea?' That's courage.
And if you're reading this and feel overwhelmed? You're not alone. I've been there. We rise together.
Steve Hesketh
January 24, 2026 AT 19:42Bro. I lost 35 lbs last year and my AHI dropped from 42 to 11. I didn't even use CPAP at first-just slept on my side and cut sugar. Now I sleep like a baby. My wife says I stopped snoring like a chainsaw.
It ain't magic. It's biology. And it's fixable.
To anyone reading this who thinks they're too tired to change? You're tired BECAUSE your body's screaming for oxygen at night. Fix the sleep, and the energy comes back. I promise.
Malvina Tomja
January 25, 2026 AT 12:00Let me be blunt: if you're obese and haven't been screened for sleep apnea, you're not just neglecting your health-you're gambling with your life. The data is irrefutable. This isn't 'maybe' or 'possibly.' It's 86% comorbidity. That's not coincidence. That's a death sentence waiting for paperwork.
And don't tell me you're 'too busy' to get tested. You're too busy breathing through your mouth at 3 a.m. while your spouse rolls away. You're too busy zoning out at work because your brain never reached REM. You're too busy paying $12,000 extra in medical bills because you refused to act.
Stop romanticizing 'natural healing.' Stop blaming stress. Stop saying 'I'll start tomorrow.' The clock is ticking. Your insulin resistance is worsening. Your blood pressure is climbing. Your heart is straining. And your sleep? It's not rest-it's a series of near-death experiences.
Get the STOP-Bang test. TODAY. Don't wait for your doctor to bring it up. They're overworked and undertrained. You are your own advocate. Print it. Bring it. Demand the sleep study. Your future self will thank you-or it won't exist at all.
Dee Monroe
January 26, 2026 AT 05:33I used to think sleep apnea was just snoring. Then I started waking up gasping. Then I started forgetting names. Then I couldn't focus at work. Then my HbA1c jumped from 6.1 to 7.8 in six months.
I didn't connect it until my sister, who's a nurse, said, 'Have you ever been tested for sleep apnea?' I laughed. I'm not fat enough. I don't snore loud enough. I'm not 'the type.'
Turns out, I'm exactly the type.
Got the CPAP. First night? I cried. Not from discomfort-from relief. I slept seven hours straight for the first time in 12 years.
Three months later, my HbA1c dropped to 6.4. I lost 11 pounds without trying. My anxiety? Gone. My energy? Like I was 25 again.
It's not a cure. It's a reset. And it's available to anyone who asks. Stop waiting for permission. Ask your doctor. Ask again. Ask until they listen. You deserve to wake up feeling alive.
Philip Williams
January 26, 2026 AT 23:07The clinical evidence presented here is robust and aligns with current guidelines from the ADA and AHA. The mechanistic link between visceral adiposity, systemic inflammation, and insulin resistance is well-documented in peer-reviewed literature, including studies from the New England Journal of Medicine and The Lancet.
Furthermore, the bidirectional relationship between sleep apnea and metabolic dysfunction is not merely correlational-it is causal, as demonstrated by randomized controlled trials showing improved insulin sensitivity following CPAP therapy.
It is imperative that primary care providers integrate routine STOP-Bang screening into standard metabolic evaluations. The cost of inaction far exceeds the cost of screening. This is public health infrastructure we are failing to build.
shubham rathee
January 27, 2026 AT 17:05Glenda Marínez Granados
January 29, 2026 AT 16:07So let me get this straight... we’ve turned human biology into a corporate flowchart?
Obesity → Diabetes → Sleep Apnea → Heart Disease → $12,300/year in bills → But hey, here’s a CPAP machine for $800 and a $500 Ozempic pen!
Meanwhile, the real problem is that we live in a world where the cheapest food is the most toxic, your job makes you too exhausted to move, and your doctor has 7 minutes to fix your soul.
So we treat symptoms with gadgets and drugs while ignoring the fact that the system is rigged?
👏👏👏 Brilliant. Just brilliant.
Now excuse me while I go cry into my 3am snack of microwaved ramen and wonder why my body betrayed me.
…and yes, I’m on CPAP. And yes, I hate the mask. But I’m alive. So… thanks? 😔
Kevin Narvaes
January 31, 2026 AT 13:55bro i just woke up from a nightmare where i was a fat person with a mask on my face and a needle in my arm and i think maybe the real problem is that we're all just... trapped in this meat prison?
like why does the body even do this to itself? is it punishment? is it evolution? did we break some cosmic rule?
i don't know. i just know i'm tired. always tired. and i keep eating. and i keep sleeping wrong. and i keep pretending i'll start tomorrow.
but maybe tomorrow never comes.
...i think i need to call my doctor.
or maybe just move to a cabin in the woods.
idk anymore.
Alex Carletti Gouvea
February 1, 2026 AT 21:04Why are we letting this narrative go unchallenged? Obesity is a Western problem caused by weak cultural values. In China, India, Africa-people don’t have this triad. They eat real food. They walk everywhere. They don’t sit in chairs all day. This isn’t biology-it’s cultural decay. We need to stop medicalizing weakness and start rebuilding discipline.
Stop blaming your genes. Stop blaming your sleep. Start lifting your butt off the couch. That’s the real solution. Not machines. Not drugs. Not screenings. Just grit.
Yuri Hyuga
February 3, 2026 AT 04:46Just read the comment from @6995-lost 35 lbs, AHI down to 11. That’s hope in motion.
To everyone else: You don’t need to lose 100 lbs. You don’t need to run marathons. You just need to start. One less soda. One walk after dinner. One question to your doctor: 'Could this be sleep apnea?'
That’s the spark.
And if you’re reading this and you’re scared? Good. Fear means you still care.
Now go make the call.
You’ve got this. 💪🌙