When you think of a generic drug, you picture a small pill that’s chemically identical to the brand-name version. But biosimilars? They’re not that simple. These are complex, living medicines-large proteins made inside living cells-that must match a reference biologic almost exactly. The catch? You can’t just copy the recipe. Even tiny changes in how they’re made can change how they work in the body. That’s why manufacturing biosimilars is one of the hardest tasks in modern medicine.
The process defines the product
Unlike small-molecule generics, where chemists can recreate the exact same compound using predictable reactions, biosimilars are made by living cells. These cells-often Chinese hamster ovary cells-are fed nutrients, kept at precise temperatures, and gently stirred in giant bioreactors. As they grow, they produce the protein drug. But no two batches are ever exactly alike. The cells respond to tiny shifts in pH, oxygen levels, or even the type of sugar in the growth medium. And that’s where the real challenge begins. The phrase “the process defines the product” isn’t just industry jargon-it’s the core truth behind biosimilar development. If you change how you feed the cells, how long you let them grow, or how you filter the final product, you change the molecule’s shape, charge, and structure. These changes might seem minor, but they can alter how the drug behaves in the body. One small difference in glycosylation-the sugar molecules attached to the protein-can make the drug clear from the bloodstream faster, reduce its ability to bind to target cells, or even trigger an immune response. Imagine trying to recreate a signature dish from a Michelin-starred restaurant without ever seeing the kitchen, tasting the food, or knowing the chef’s techniques. That’s what biosimilar developers face. They have the final product in hand, but not the recipe. They must reverse-engineer thousands of subtle characteristics using advanced analytical tools to map the reference product’s “molecular fingerprint.” Only then can they design a manufacturing process that gets as close as humanly possible.Glycosylation: the silent wildcard
Glycosylation is one of the most difficult aspects to control. These sugar chains stick out from the protein like branches on a tree. Their length, branching pattern, and composition vary based on culture conditions, cell line health, and even the time of year. A single change in glycosylation can turn a therapeutic protein into a less effective-or even dangerous-version of itself. For example, if a monoclonal antibody used to treat cancer has too few sialic acid residues on its glycans, the immune system might attack it too quickly. Too many, and it might not bind tightly enough to cancer cells. The reference product has a specific glycosylation profile that’s been proven safe and effective over years of clinical use. The biosimilar must match it within strict limits-usually within 5% variability. But achieving that consistency across hundreds of batches, over years of production, is like trying to hit a moving target with your eyes closed. To tackle this, manufacturers use high-resolution mass spectrometry, capillary electrophoresis, and other cutting-edge tools to analyze glycan structures down to the atomic level. But even with the best tech, it takes years of trial and error to fine-tune the process. One company spent nearly three years adjusting feed rates and dissolved oxygen levels just to stabilize glycosylation in a single biosimilar candidate.Scaling up without losing control
Getting a biosimilar to work in a 10-liter lab bioreactor is one thing. Getting it to work in a 10,000-liter commercial tank is another. At small scale, you can control every variable with precision. At large scale, mixing becomes uneven. Oxygen doesn’t distribute evenly. Temperature gradients form. Cells in one corner get more nutrients than those in another. These physical differences change how the cells behave-and therefore, the protein they produce. Manufacturers must map out how every parameter scales. Stirring speed? It can’t just be increased proportionally. Oxygen transfer rates change with tank geometry. Feeding strategies that worked in a 500-liter tank might cause cell death in a 5,000-liter one. Many companies have lost entire batches because they assumed a linear scale-up would work. That’s why modern biosimilar plants use advanced modeling software and real-time sensors to monitor conditions. Process analytical technology (PAT) lets them track pH, dissolved oxygen, and metabolite levels as the batch runs. If something drifts, the system adjusts automatically. Still, it’s expensive. Building a facility with this level of monitoring can cost over $500 million.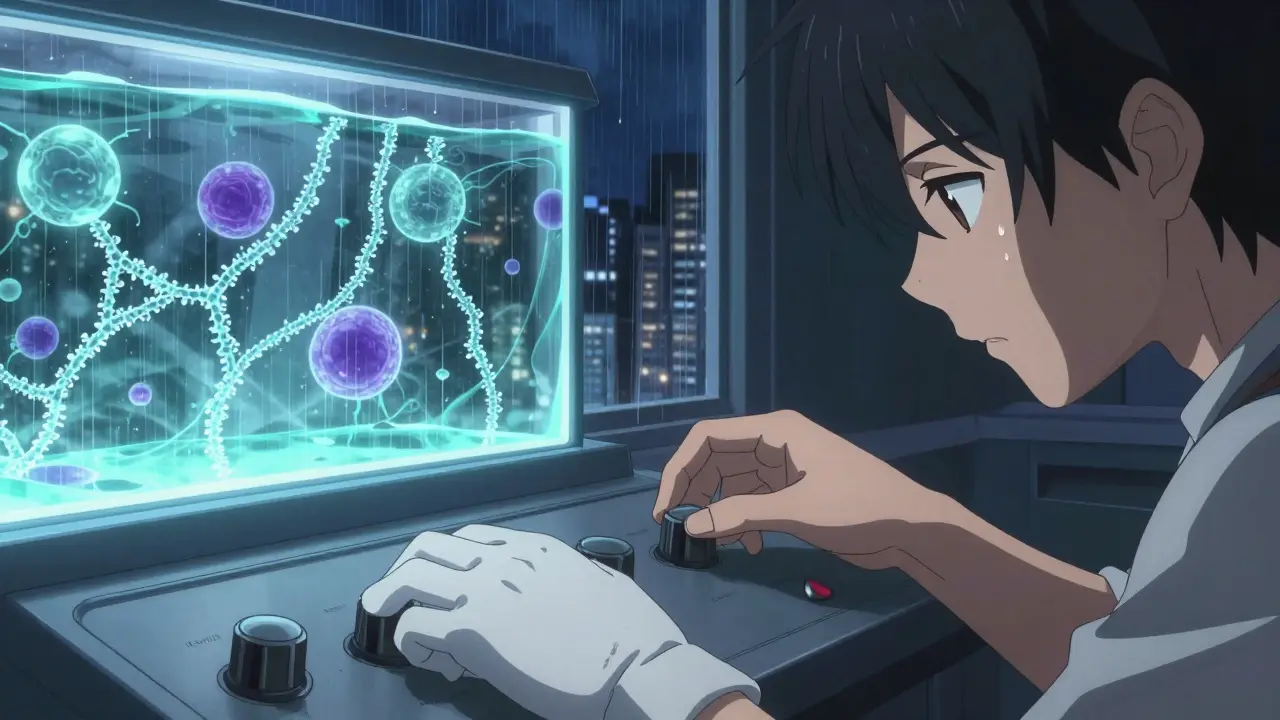
The cold chain nightmare
Biosimilars don’t just need careful production-they need careful handling from the moment they’re made. Most are proteins, and proteins are fragile. Heat, vibration, light, even too much shaking can break them apart. That’s why the cold chain-the network of refrigerated storage and transport-is critical. One biosimilar manufacturer lost $12 million in product last year because a refrigerated truck’s temperature sensor failed during a 48-hour transport. The batch was still within legal temperature limits, but the protein had degraded enough to fail quality tests. The company had to recall the entire shipment. That’s not rare. In fact, 1 in 6 biosimilar shipments experience some kind of cold chain issue. To fix this, companies are switching to single-use containers and smart packaging with embedded temperature loggers. Some even use blockchain to track every step of the journey. But these solutions add cost-and complexity. Smaller manufacturers struggle to afford them, putting them at a disadvantage against big players.Regulatory maze
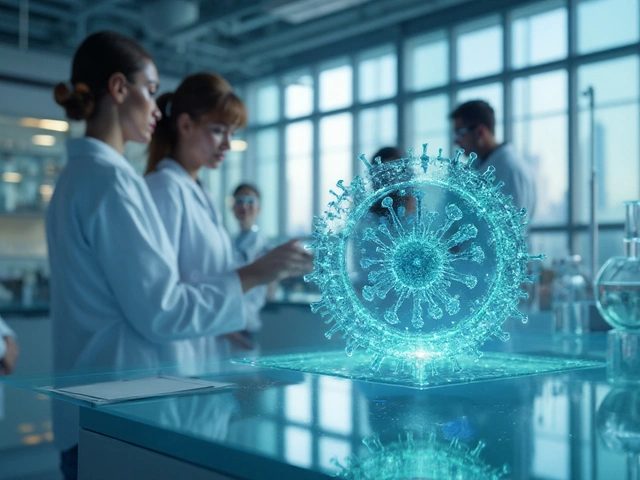
Getting a biosimilar approved isn’t like getting a generic approved. The FDA and EMA don’t just want proof that it’s similar-they want proof that it’s as safe and effective as the original. That means extensive analytical data, animal studies, and sometimes even clinical trials. The regulatory bar keeps rising. In 2023, the FDA updated its guidance to require more detailed comparisons of post-translational modifications, including glycosylation, deamidation, and oxidation. Developers now need to show they can control these variables consistently-not just in one batch, but across every batch they’ll ever make. And it’s not just one agency. Each country has its own rules. The EU might accept a reduced clinical trial program if analytical data is strong. The FDA might demand a full head-to-head trial. China has its own pathway. Navigating this is like solving a different puzzle in every country.
Technology is changing the game
The industry is fighting back with new tools. Single-use bioreactors are replacing stainless steel tanks. They eliminate cleaning validation, reduce contamination risk, and let manufacturers switch between products faster. Automation is cutting human error-robots now handle filling and labeling in cleanrooms, reducing the chance of mistakes. Artificial intelligence is helping too. Machine learning models analyze years of manufacturing data to predict which process changes will cause quality issues before they happen. One company reduced batch failures by 40% in two years by using AI to adjust feed strategies in real time. Continuous manufacturing is the next frontier. Instead of making one batch at a time, some companies are moving toward a steady flow of production-like a pipeline. This reduces variability and improves consistency. But it’s still early. Only a handful of biosimilars are made this way today.Who can afford to play?
The global biosimilars market is projected to hit $58 billion by 2030. But only a few dozen companies have the expertise, capital, and infrastructure to compete. The cost to develop and launch a single biosimilar? Often over $100 million. The time? At least seven years. Smaller players are getting squeezed. Many lack the analytical labs, automation systems, or regulatory teams needed to keep up. Some are turning to partnerships-licensing technology from bigger firms or outsourcing production. Others are focusing on simpler biosimilars first, like insulin or growth hormones, before tackling complex ones like bispecific antibodies. The ones who win? Those who treat manufacturing not as a cost center, but as the core of their product. They invest in process understanding, not just product testing. They build flexibility into their plants. They train their teams to think like scientists, not just operators.What’s next?
The future of biosimilars lies in smarter processes, not just cheaper ones. As more complex biologics lose patent protection-like antibody-drug conjugates and fusion proteins-the manufacturing challenges will only grow. But so will the demand. Patients need affordable options. Health systems need cost savings. The companies that succeed won’t be the ones with the biggest budgets. They’ll be the ones who truly understand that a biosimilar isn’t just a copy. It’s a re-creation. And re-creating a living molecule, perfectly, every time, is one of the most difficult feats in science.Why can’t biosimilars be exact copies like generic drugs?
Biosimilars are made from living cells, not chemicals. Even tiny changes in the manufacturing process-like temperature or nutrient mix-can alter the protein’s structure. Generics are small molecules made with predictable chemical reactions, so they can be identical. Biosimilars are large, complex proteins that can’t be copied exactly, only closely matched.
What’s the biggest technical hurdle in biosimilar manufacturing?
Glycosylation-the addition of sugar molecules to the protein-is the most difficult to control. These sugars affect how the drug works in the body, and they’re highly sensitive to production conditions. Matching the reference product’s exact glycan profile requires years of fine-tuning and advanced analytical tools.
Why is scale-up so challenging for biosimilars?
In small bioreactors, conditions are easy to control. In large ones, mixing, oxygen levels, and temperature become uneven. Cells in different parts of the tank grow differently, leading to inconsistent protein quality. Scaling isn’t just about size-it’s about preserving the exact biological environment that makes the protein work.
How do regulators ensure biosimilars are safe?
Regulators require deep analytical comparisons of hundreds of quality attributes, plus clinical studies to prove safety and effectiveness. They don’t just check if the molecule looks similar-they test how it behaves in the body. This includes immune response, clearance rates, and binding strength to target cells.
Are biosimilars cheaper to make than originator biologics?
Not necessarily. While biosimilars cost less to develop than new biologics, manufacturing them is still extremely expensive. The equipment, testing, and regulatory burden often make the production costs comparable to the original. Savings come from competition, not lower production costs.
What role does automation play in biosimilar manufacturing?
Automation reduces human error and contamination risk. Robots handle filling, labeling, and testing in cleanrooms. Closed, automated systems also improve consistency by minimizing manual interventions. This is especially critical for sensitive products where even a small mistake can ruin a whole batch.
Can small companies make biosimilars?
It’s extremely difficult. The capital required for analytical labs, automated systems, and compliant facilities is prohibitive for most small firms. Many now partner with contract manufacturers or focus on simpler biosimilars like insulin. Only a handful of small companies have successfully launched complex biosimilars.
What’s the difference between a biosimilar and a biobetter?
A biosimilar aims to match the reference product exactly in safety and effectiveness. A biobetter is intentionally modified to improve on the original-like longer-lasting effects or fewer side effects. Biobetters are treated as new drugs, not biosimilars, and require full clinical trials.







Malikah Rajap
January 18, 2026 AT 21:12Wow, I just read this and I’m sitting here with my tea, thinking-how is this even possible? We’re asking living cells to be perfect little factories, and we’re mad when they sneeze and mess up the glycosylation? It’s like expecting a Picasso to paint the same brushstroke 500 times… while blindfolded… in a hurricane.
But also-why are we so obsessed with copying? Isn’t the real win making something better? Like, if we can tweak these proteins to last longer or have fewer side effects, why are we stuck in this ‘match exactly’ loop?
I mean, I get the regs, I do-but this feels like trying to recreate your grandma’s soup by analyzing the steam.
Aman Kumar
January 19, 2026 AT 18:13The fundamental epistemological failure of the biosimilar paradigm lies in its ontological misapprehension of biologics as reproducible entities. The very notion that a protein’s post-translational modifications can be standardized across biological systems is a reductive fallacy rooted in Cartesian mechanicism-a paradigm utterly incompatible with the emergent complexity of living systems.
Glycosylation heterogeneity isn’t a ‘challenge’-it’s a biological truth. To demand homogeneity is to impose industrial logic upon a phenomenon that evolved for variability. This isn’t manufacturing. It’s bio-surrealism.
And don’t get me started on the regulatory theater. The FDA’s ‘5% variability’ is a placebo metric. It’s not science-it’s compliance theater dressed in mass spectrometry.
Valerie DeLoach
January 21, 2026 AT 06:22I love how this post breaks down the science without jargon overload. It’s easy to forget that behind every biosimilar is a team of scientists who’ve spent years chasing invisible sugar chains.
But I also think we need to talk about who gets left out. The $500M facilities, the AI systems, the global regulatory teams-these aren’t just technical hurdles. They’re economic gatekeepers.
What if we built open-source analytical frameworks? What if small labs could share glycan data in a neutral, anonymized repository? We don’t need more patents-we need more collaboration.
And honestly? The cold chain failures? That’s a global justice issue. A patient in rural India deserves the same stable medicine as someone in Boston. We’re not just making drugs-we’re making equity.
Josh Kenna
January 21, 2026 AT 08:47okay so i just read this and i think i might have cried a little? like-imagine spending 3 years just trying to get the sugar right on one protein? that’s insane. and then the truck breaks and $12M is gone? that’s not a business, that’s a horror movie.
but also-why do we keep acting like this is normal? we’re asking cells to be robots, and then punishing them when they act like living things? we need to stop pretending we’re in control here.
also-i’m not a scientist but i think we should just call them ‘biocopies’ and be done with it. ‘biosimilar’ sounds like a legal loophole.
Erwin Kodiat
January 22, 2026 AT 02:38Honestly? This is one of the most fascinating things I’ve read all year. It’s like watching a ballet where every dancer is made of jelly and the music changes every 20 minutes.
And yet-people still think generics and biosimilars are the same. No. One’s a photocopy. The other’s a live orchestra trying to recreate a symphony from a single recording.
Big props to the teams doing this work. We don’t celebrate them enough. They’re not just making medicine-they’re doing molecular origami with a blindfold on.
Jackson Doughart
January 23, 2026 AT 14:24The precision required to replicate a biologic’s molecular architecture is not merely technical-it is metaphysical. Each glycan branch, each deamidation site, each disulfide bond represents a cascade of biological intention.
When we speak of ‘matching’ a reference product, we are not comparing molecules-we are attempting to resurrect a living signature. The notion that this can be achieved through industrial means is, at its core, a profound anthropocentric delusion.
And yet-we persist. Because the alternative is denying patients access. And that, perhaps, is the only moral imperative that justifies this Herculean folly.
Lydia H.
January 25, 2026 AT 02:09Okay but-what if we stopped trying to copy and started evolving? Like, what if instead of matching the original, we made a version that’s *better* for people with autoimmune conditions? Or less likely to cause infusion reactions?
Why are we stuck in ‘copy mode’? Isn’t the whole point of biologics that they’re alive? Maybe we should let them live a little differently.
Also, I just realized-we’re treating cells like they’re machines, but they’re more like tiny, grumpy artists. Maybe we need to stop micromanaging and start listening.
Phil Hillson
January 25, 2026 AT 03:33This whole thing is a scam
Big Pharma invented biosimilars so they could keep charging $200K a year but call it ‘affordable’
They don’t care if the sugar chains are perfect
They just want you to think it’s the same
And regulators? They’re in the pocket
Read the patents-half the ‘innovations’ are just packaging tricks
Also-why do we still use Chinese hamster cells? That’s 1980s tech
Someone’s hiding something
Jacob Hill
January 25, 2026 AT 18:32Can I just say-this is one of the most beautifully written explanations I’ve ever read? I’m not in biotech, but I feel like I understand now why my cousin’s insurance denied her biosimilar last year.
It’s not about cost. It’s about control. And control? That’s the real drug here.
Also-has anyone considered that maybe we don’t need to match *exactly*? Maybe we just need to match *well enough*? Like, if it works, and it’s safe, and it’s cheaper-why are we still sweating the 4.8% glycan difference?
Just saying.
Lewis Yeaple
January 27, 2026 AT 15:11The assertion that biosimilars are ‘not exact copies’ is scientifically inaccurate. All biologics exhibit inherent heterogeneity; therefore, the reference product itself is not a single molecular entity, but a population of variants. The biosimilar, by definition, must demonstrate comparability across the same distributional parameters.
Thus, the notion of ‘exact copy’ is a misnomer perpetuated by lay media. The regulatory framework does not require identity-it requires equivalence within statistically defined boundaries.
Failure to comprehend this distinction undermines the entire scientific discourse.
sujit paul
January 28, 2026 AT 16:25Did you know that the Chinese hamster ovary cells used in biosimilar production are not native to China? They were originally harvested from a lab in Switzerland in 1957, then modified by American biotech firms under classified DARPA contracts?
And the glycosylation patterns? They were reverse-engineered from a 1998 patent that was never meant to be public. The ‘reference product’ was actually modified by a single scientist in Germany who later vanished.
That’s why every biosimilar fails at scale-it’s not the process. It’s the origin.
The truth is hidden. The cells are listening. And they remember.
Christi Steinbeck
January 29, 2026 AT 07:41Y’all are overthinking this. The real problem? We treat biosimilars like they’re magic. They’re not. They’re just protein. And protein? It’s just amino acids. We’ve been making protein since we learned to boil soup.
Stop romanticizing the glycosylation. Stop worshipping the bioreactor. Just make it work. Test it. If it saves lives, it’s good.
And if it costs half as much? Even better.
We don’t need AI. We don’t need $500M plants. We need people who care more about patients than patents.