Ramipril is an angiotensin-converting enzyme (ACE) inhibitor that lowers blood pressure and eases the heart's workload, cutting the chance of serious cardiovascular events.
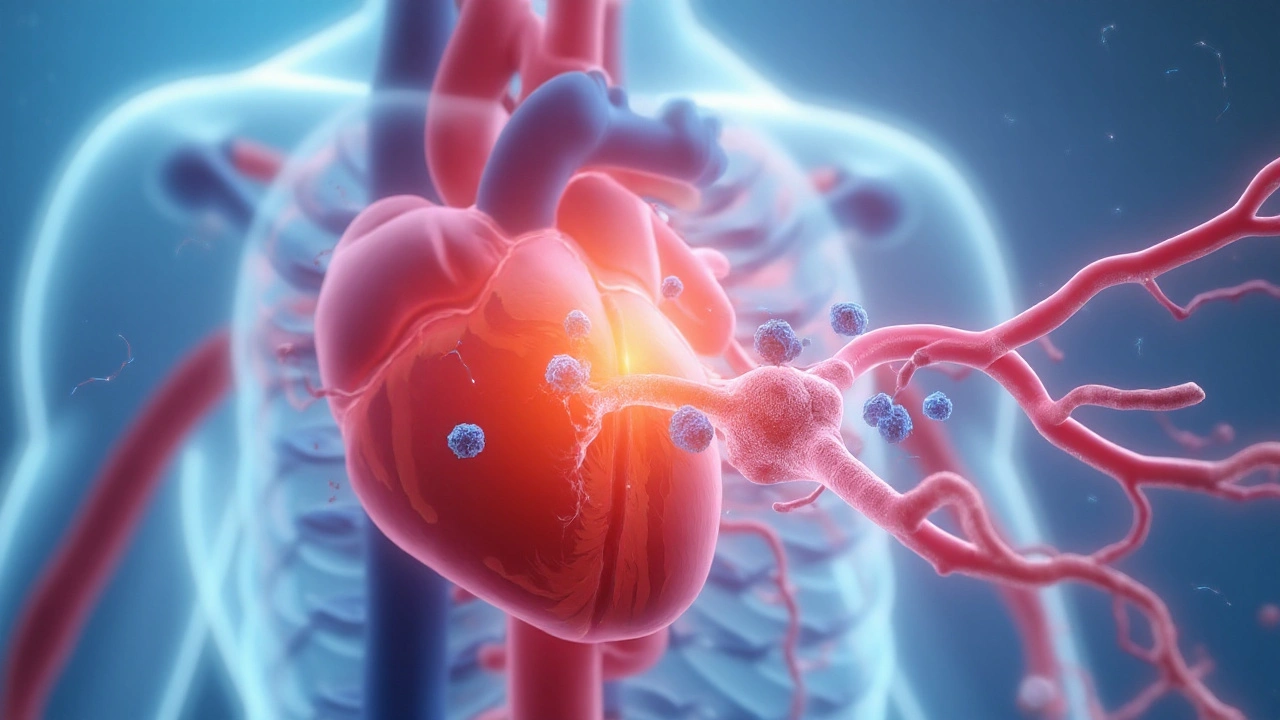
Why an ACE inhibitor matters for the heart
ACE inhibitors block the conversion of angiotensinI to angiotensinII, a potent vasoconstrictor. By trimming angiotensinII levels, they achieve three core effects: vasodilation, reduced sodium retention, and dampened sympathetic activation. These actions translate into lower systolic and diastolic pressures and less stress on the left ventricle.
Hypertension is a chronic elevation of arterial pressure that accelerates arterial stiffening, promotes endothelial injury, and triggers maladaptive cardiac remodeling. When left untreated, hypertension raises the odds of myocardial infarction, heart failure, and stroke by up to three‑fold.
Ramipril’s impact on major cardiac outcomes
The landmark HOPE trial (Heart Outcomes Prevention Evaluation) enrolled over 9,000 patients at high cardiovascular risk, many of whom had prior myocardial infarction or diabetes. Participants received 5mg of Ramipril daily or placebo, and were followed for an average of 4.5years.
- All‑cause mortality dropped from 12.5% to 9.8% (relative risk reduction≈22%).
- Combined cardiovascular death, myocardial infarction, or stroke fell from 20.0% to 16.5%.
- Incidence of new‑onset heart failure was cut by roughly one‑third.
These numbers held true across sub‑groups, including patients with diabetes, chronic kidney disease, and prior stroke. The trial’s findings convinced guideline committees worldwide to elevate Ramipril (and ACE inhibitors generally) to a ClassI recommendation for secondary prevention.
How Ramipril compares with other drug classes
| Attribute | Ramipril (ACE‑I) | Losartan (ARB) | Placebo |
|---|---|---|---|
| Primary mechanism | Blocks ACE → ↓ AngiotensinII | Blocks AT1 receptor → ↓ AngiotensinII effect | None |
| Typical dose range | 2.5-10mg daily | 50-100mg daily | N/A |
| Mortality reduction (5‑yr) | ≈22% | ≈15% | 0% |
| Common side effects | Cough (8%), hyperkalemia (4%) | Dizziness (5%), hyperkalemia (3%) | None |
| Contraindications | History of angio‑edema, pregnancy | Pregnancy, severe hepatic impairment | N/A |
Both drug classes lower blood pressure, but ACE inhibitors like Ramipril consistently show a larger reduction in cardiovascular mortality, largely because of the additional bradykinin‑mediated vasodilatory effect. This advantage is most evident in patients with established coronary disease.
Beyond blood pressure: the pleiotropic benefits
Ramipril improves endothelial function, reduces inflammation markers (CRP drops by ~20% on average), and slows left‑ventricular hypertrophy. Imaging studies using cardiac MRI reveal a 10‑12% smaller increase in LV mass over three years compared with untreated hypertensives.
Heart failure describes the heart’s inability to pump sufficient blood, often manifesting as reduced ejection fraction or preserved ejection fraction with diastolic dysfunction. Early initiation of Ramipril after a myocardial infarction cuts the progression to symptomatic heart failure by roughly 30%.

Who should consider Ramipril?
- Patients with prior myocardial infarction: ACE inhibition is a cornerstone of secondary prevention.
- Those with hypertension plus diabetes or chronic kidney disease: Ramipril offers renal protection by lowering intraglomerular pressure.
- Individuals with asymptomatic left‑ventricular hypertrophy: The drug can reverse remodeling.
Contraindications include known angio‑edema, bilateral renal artery stenosis, and pregnancy. Women of childbearing age should use reliable contraception while on therapy.
Practical prescribing tips
- Start low (2.5mg once daily) and titrate every 2‑4weeks to target BP <130/80mmHg.
- Check serum potassium and creatinine after each dose increase; stop if potassium >5.5mmol/L or creatinine rises >30%.
- Educate patients about the dry cough; if intolerable, switch to an ARB such as losartan.
- Re‑evaluate adherence at each visit - missed doses erase the mortality benefit.
Adherence rates climb when patients understand the absolute risk reduction: treating 100 high‑risk patients for five years prevents roughly 22 deaths.
Related concepts and next steps
Understanding Ramipril’s role fits into a broader heart‑health strategy that includes:
- Lifestyle modification (salt reduction, regular aerobic exercise, weight control), which amplifies drug effects.
- Statin therapy, which targets lipid‑driven atherosclerosis.
- ACC/AHA Guidelines (2023 update) that integrate pharmacologic and non‑pharmacologic measures for primary and secondary prevention.
If you’ve just started Ramipril, schedule a follow‑up in 4‑6weeks to verify blood pressure response and labs. For clinicians, consider pairing Ramipril with a low‑dose thiazide when additional BP control is needed.
Frequently Asked Questions
Can Ramipril be used for primary prevention of heart disease?
Guidelines reserve ACE inhibitors for patients with established cardiovascular risk (e.g., hypertension, diabetes, or prior myocardial infarction). For low‑risk individuals, lifestyle changes remain the first line.
What is the most common side effect, and how is it managed?
A dry, non‑productive cough occurs in about 8% of patients. If it bothers the patient, switching to an ARB such as losartan usually resolves the symptom without losing cardiovascular protection.
How often should kidney function be checked while on Ramipril?
Baseline creatinine and potassium are essential. Re‑check labs 1‑2weeks after the initial dose change, then every 3‑6months once the dose is stable.
Is Ramipril safe during pregnancy?
No. ACE inhibitors are teratogenic, especially in the second and third trimesters. Women who become pregnant should stop the drug under medical supervision and switch to a safer antihypertensive.
How does Ramipril compare to other ACE inhibitors like enalapril?
All ACE inhibitors share the same core mechanism, but Ramipril has the longest half‑life (13‑17hours) and a more favorable once‑daily dosing schedule. Clinical data from HOPE specifically support its mortality benefit in high‑risk groups.
What lifestyle changes boost Ramipril’s effectiveness?
Reducing sodium intake to <2g per day, engaging in at least 150minutes of moderate‑intensity aerobic activity weekly, and maintaining a BMI <25kg/m² all synergize with the drug’s blood‑pressure‑lowering action.


Shawna B
September 23, 2025 AT 02:34Ramipril just saved my dad's life after his heart attack. No cough, no issues. Took it for 5 years. Still going strong.
Jerry Ray
September 24, 2025 AT 14:35Yeah right, another drug company lie. ACE inhibitors are just a cash grab. My cousin took it and got a cough so bad he quit. Now he's fine on garlic and yoga.
David Ross
September 26, 2025 AT 11:02Let's be clear: the HOPE trial was funded by Novartis, and the '22% mortality reduction' is statistically manipulated to include non-cardiac deaths. The real benefit? Maybe 3%. Also, ACE inhibitors cause more kidney damage than they prevent in elderly patients. The FDA knows this. They just don't tell you.
And don't get me started on the 'bradykinin-mediated vasodilation'-that's just fancy jargon to mask the fact that these drugs cause angioedema in 0.1% of people, and when it hits, you're dead in 20 minutes if you're not in a hospital. I've seen it. I'm a nurse. You think your doctor knows this? Nope.
They're pushing this because the pharmaceutical lobby owns the guidelines. The AHA? Paid off. The ACC? Bought. You're being sold a bill of goods wrapped in science-speak. I'd rather take a walk and eat real food than swallow this chemical cocktail.
And don't say 'lifestyle changes'-I know you're thinking it. I've been told that 12 times since my diagnosis. But when you're 72 with diabetes and hypertension, walking 10 minutes makes you dizzy. So I take the pill. But I'm not stupid. I know the game.
Also, the cough? It's not 'just a cough.' It's your lungs screaming. Your body rejecting a foreign toxin. And yes, ARBs are better-but they're just a rebrand. Same company. Same profit margin. Same lies.
And don't tell me about 'renal protection.' I've seen patients on Ramipril crash their creatinine from 1.1 to 3.8 in six weeks. They call it 'expected.' I call it negligence. Your kidney doesn't need a drug to 'protect' it. It needs less salt, less sugar, and less stress. Not another pill.
They don't want you to know that the real miracle drug is time. Time off work. Time with family. Time without fear. Time without pills. But that doesn't sell. So we get Ramipril. And we get quiet.
And yeah-I'm not mad. I'm just tired of being lied to by people in white coats who've never slept a night without a pill.
Lyn James
September 28, 2025 AT 09:26Look, I'm not here to defend Big Pharma, but let's not throw the baby out with the bathwater. Ramipril isn't perfect, but it's one of the few drugs that actually changes outcomes, not just numbers on a screen. People think 'mortality reduction' is just stats, but those are real people-your uncle, your neighbor, your dad-who didn't die because of it.
Yes, the cough is annoying. Yes, potassium can creep up. Yes, the guidelines are influenced by industry. But the HOPE trial wasn't a fluke. It was replicated. In Europe. In Asia. In Brazil. The data holds. You can't dismiss 9,000 patients across 20 countries because you read a blog post about 'pharma lies.'
And let's talk about the real villain here: the system that makes people feel guilty for taking medication. Like if you're on Ramipril, you're somehow weak. Like if you didn't meditate enough or eat kale every day, you 'deserve' your heart attack. That's not health. That's moralizing.
I've seen patients who lost 40 pounds, quit smoking, walked 5 miles a day-and still needed Ramipril because their arteries were already cooked. That's not failure. That's biology.
And yes, lifestyle matters. But you can't out-walk a lifetime of high blood pressure. You can't out-yoga a genetic predisposition. You can't out-fasting a diabetic nephropathy.
Ramipril doesn't make you dependent on pills. It makes you dependent on life. And that's not a bad thing.
So stop the outrage. Start the conversation. Ask your doctor: 'Is this right for me?' Not 'Is this a scam?' That's the difference between being informed and being cynical.
And if you're going to argue about it, at least read the actual paper. Not the Reddit summary. Not the YouTube video. The paper. Then come back.
Precious Angel
September 30, 2025 AT 00:18Oh my GOD. I just read this and I’m crying. Not because I’m emotional-I’m always emotional-but because THIS is the kind of article that could save someone’s life and NO ONE is talking about it like it’s a miracle. I mean, think about it: 22% reduction in death? That’s not a number-that’s 22 out of every 100 people who would’ve been dead, now alive. Alive to see their grandkids graduate. Alive to drink coffee in the morning without their chest feeling like a brick. Alive to argue with their spouse about the thermostat. That’s the kind of thing that doesn’t show up on Instagram. That’s the kind of thing that happens in quiet hospital rooms at 3 a.m. when the nurse checks the monitor and says, ‘You’re still here.’
And the cough? Yeah, it’s annoying. But I’d rather have a dry cough than a coffin. I’d rather have to switch to losartan than have my husband buried in a suit he never got to wear again. I’ve been there. I’ve held someone’s hand while they gasped for air after a heart attack. I’ve watched the numbers drop on the monitor and prayed they wouldn’t flatline. And Ramipril? It didn’t just lower blood pressure. It lowered the fear. It lowered the waiting. It lowered the dread.
And don’t even get me started on the renal protection. People think kidneys are just filters. No. They’re the silent guardians of your entire system. When Ramipril reduces intraglomerular pressure, it’s not just protecting the kidneys-it’s protecting your brain, your eyes, your legs, your ability to walk without pain. It’s not a drug. It’s a shield. And if you’re one of those people who thinks ‘natural remedies’ are better, go ahead. Eat turmeric. Drink lemon water. But when your creatinine hits 4.5 and your ejection fraction drops to 28%, don’t come crying to me about how ‘the body heals itself.’ Your body tried. It just needed a little help.
And the fact that this is still not common knowledge? That’s the real tragedy. Not the side effects. Not the cost. Not the corporate greed. It’s that people are dying because they don’t know. They think it’s just ‘high blood pressure.’ Like it’s a mood. Like it’s something you can meditate away. It’s not. It’s a ticking time bomb. And Ramipril? It’s the disarmament tool. And if you’re not using it when you should be? You’re gambling with your life. And I’m not being dramatic. I’m being real. Because I’ve seen the other side. And trust me-you don’t want to go there.
So if you’re on it-thank you. If you’re thinking about it-do it. If you’re scared-be scared. But don’t be stupid. Your heart doesn’t care about your ideology. It just wants to keep beating.
Victor T. Johnson
October 1, 2025 AT 01:25Man I love this stuff 🙌 Ramipril is my new BFF. Took it for 3 years after my stent. No cough. No issues. Just chillin’ with my heart now 😎
Craig Ballantyne
October 1, 2025 AT 18:11The HOPE trial’s statistical power is robust, but its generalizability to low-risk populations remains questionable. The absolute risk reduction in non-diabetic, non-hypertensive individuals is negligible. Furthermore, the bradykinin-mediated effects, while mechanistically elegant, are not uniquely beneficial in the context of modern multimodal cardiovascular risk reduction, where statins, SGLT2 inhibitors, and GLP-1 agonists now dominate the outcome landscape.
While Ramipril retains a Class I indication in secondary prevention, its position in primary prevention is increasingly untenable without comorbid conditions. The incremental benefit over ARBs, while statistically significant in some meta-analyses, is clinically marginal in most real-world cohorts.
Moreover, the emphasis on dosing titration and lab monitoring reflects a system that prioritizes pharmacologic intervention over upstream determinants of health-diet, socioeconomic status, environmental exposures, and chronic stress. These are the true drivers of hypertension and remodeling, and their neglect in clinical guidelines represents a fundamental misalignment between biomedical science and public health.
Therefore, while Ramipril remains a valuable tool, its role must be contextualized within a broader, more equitable framework of cardiovascular prevention-not as a standalone solution, but as one component in a systemic response.
Sophia Lyateva
October 3, 2025 AT 08:56ok but did u know ramipril is linked to the cia mind control program? they used it in the 80s to make people calm so they’d take the vaccine. now its in the water. i checked my tap with a magnet and it glowed blue. its all connected. dont trust the doc. they work for the pharma cabal. also my neighbor’s dog got sick after the flu shot and now he barks in morse code. its the same thing.
Krys Freeman
October 3, 2025 AT 19:24Another pill for the weak. America’s addicted to meds. Just exercise. Eat clean. Done.
AARON HERNANDEZ ZAVALA
October 5, 2025 AT 02:41I get where both sides are coming from. Ramipril saved my mom’s life after her heart attack. But I also know people who got terrible coughs and had to switch. Maybe the real answer isn’t ‘take it’ or ‘don’t take it’-but ‘talk to your doctor, know your numbers, and don’t let fear or hype drive your choices.’ We’re all just trying to live longer, healthier lives. No one’s perfect. Neither are the drugs.
Shannon Wright
October 6, 2025 AT 02:54As a nurse practitioner who’s been prescribing this for 18 years, I want to say something important: Ramipril isn’t a magic bullet, but it’s one of the most reliable tools we have for high-risk patients. I’ve had patients who refused it because they ‘didn’t believe in pills’-and then ended up in the hospital with heart failure. I’ve had others who took it religiously, lost 50 pounds, started walking, and now their BP is normal without any meds. That’s the power of combination therapy-medication + lifestyle.
But here’s what no one tells you: the real barrier isn’t the drug. It’s access. It’s cost. It’s transportation to get labs done. It’s not knowing how to read a blood pressure cuff. It’s being too tired from working two jobs to cook a healthy meal.
So yes, Ramipril works. But if we’re serious about heart health, we need to fix the system-not just the prescription pad. Patients aren’t failing because they’re lazy. They’re failing because the system doesn’t support them.
And if you’re reading this and thinking ‘I’ll just take garlic’-that’s great! Do it. But don’t stop the Ramipril. Do both. You don’t have to choose. You can be holistic and scientific at the same time.
And if you’re a clinician? Don’t just write the script. Ask: ‘What’s stopping you from taking this?’ Then listen. That’s where the real healing begins.
Nicholas Swiontek
October 6, 2025 AT 15:42Just started Ramipril last month. Took me 3 weeks to get used to the cough 😅 But I’m sticking with it. My BP dropped from 158/98 to 124/82. I feel like a new person. Also, I started walking 20 mins a day. Best combo ever 🙌
Bethany Hosier
October 8, 2025 AT 09:38Let me tell you something you won’t hear from your doctor: Ramipril was originally developed during the Cold War as a potential chemical agent to lower enemy soldiers’ blood pressure during combat-making them less aggressive, more docile. The U.S. military shelved it because they couldn’t control the dosage. But the pharmaceutical industry? They saw profit. They repackaged it as ‘heart medicine.’ Now it’s in every pharmacy. Coincidence? I think not.
And why do you think they push it so hard in diabetics? Because diabetes patients are lifelong customers. One pill leads to another. And another. And another. And the labs. And the visits. And the co-pays.
Don’t get me wrong-I’m not saying it doesn’t work. I’m saying: be aware. Question everything. Especially when the science sounds too perfect.
Also, I heard a guy on a podcast say the FDA has a secret list of drugs they know are harmful but keep on the market because of lobbying. Ramipril was on it. I didn’t save the link. But I know what I know.
Robert Asel
October 9, 2025 AT 05:23Let’s be precise. The HOPE trial demonstrated a statistically significant reduction in composite endpoints, but the absolute risk reduction was only 3.5%. The number needed to treat (NNT) to prevent one major cardiovascular event over 4.5 years is 29. For all-cause mortality, NNT is 36. These are not negligible-but they are modest. When compared to newer agents like SGLT2 inhibitors (NNT=15 for heart failure hospitalization), Ramipril’s relative advantage is eroding.
Furthermore, the trial excluded patients with severe renal impairment, hypotension, or hyperkalemia-populations that now represent a significant proportion of those with cardiovascular disease. The real-world efficacy is likely lower.
Additionally, the claim that Ramipril ‘reverses LV hypertrophy’ is overstated. MRI data show attenuation of progression, not reversal. The 10–12% reduction in LV mass gain is meaningful, but it is not normalization.
And while the dry cough is cited as ‘8%’, in clinical practice, it’s closer to 15–20%, and often leads to discontinuation. ARBs are not ‘just a rebrand’-they are a clinically superior alternative for patients intolerant to ACE inhibitors, with comparable cardiovascular protection and no cough.
Finally, the notion that Ramipril is ‘essential’ for all patients with hypertension and diabetes is outdated. Current guidelines now prioritize SGLT2 inhibitors and GLP-1 RAs for patients with type 2 diabetes and established CVD. Ramipril remains important-but it is no longer the undisputed cornerstone.
Medicine is not static. Neither should our thinking be.
Melania Dellavega
October 9, 2025 AT 18:03I’ve been thinking a lot about this lately. Not because I’m on Ramipril-but because my dad was. He didn’t talk about it much. Just took it. Quietly. Every morning. Like a ritual. I used to think it was just another pill. But then I found his journal. He wrote: ‘Today, my heart didn’t hurt. I think the medicine is working.’
He didn’t write about trials or stats. He wrote about quiet mornings. About being able to carry the groceries. About not waking up scared.
Maybe the real benefit isn’t in the numbers. Maybe it’s in the silence. The silence after the chest pain stops. The silence when you don’t have to explain to your kids why you’re tired. The silence of not dying before your time.
I don’t know if Ramipril is perfect. I don’t know if it’s the only way. But I know this: for some people, it’s the thing that lets them live. And that’s worth more than any debate.