Drug-Induced Lung Damage Risk Assessment Tool
This tool assesses your risk of developing drug-induced pulmonary fibrosis based on medications you're taking and other factors. It's designed to help you understand potential risks and encourage conversations with your healthcare provider.
Do you experience any of these symptoms?
Most people assume that if a doctor prescribes a medication, it’s safe. But some drugs don’t just treat illness-they can quietly scar your lungs. Drug-induced pulmonary fibrosis is one of those hidden dangers. It’s not rare. It’s not theoretical. It’s happening right now to people taking common pills for heart problems, arthritis, infections, and even cancer. And many don’t realize what’s happening until it’s too late.
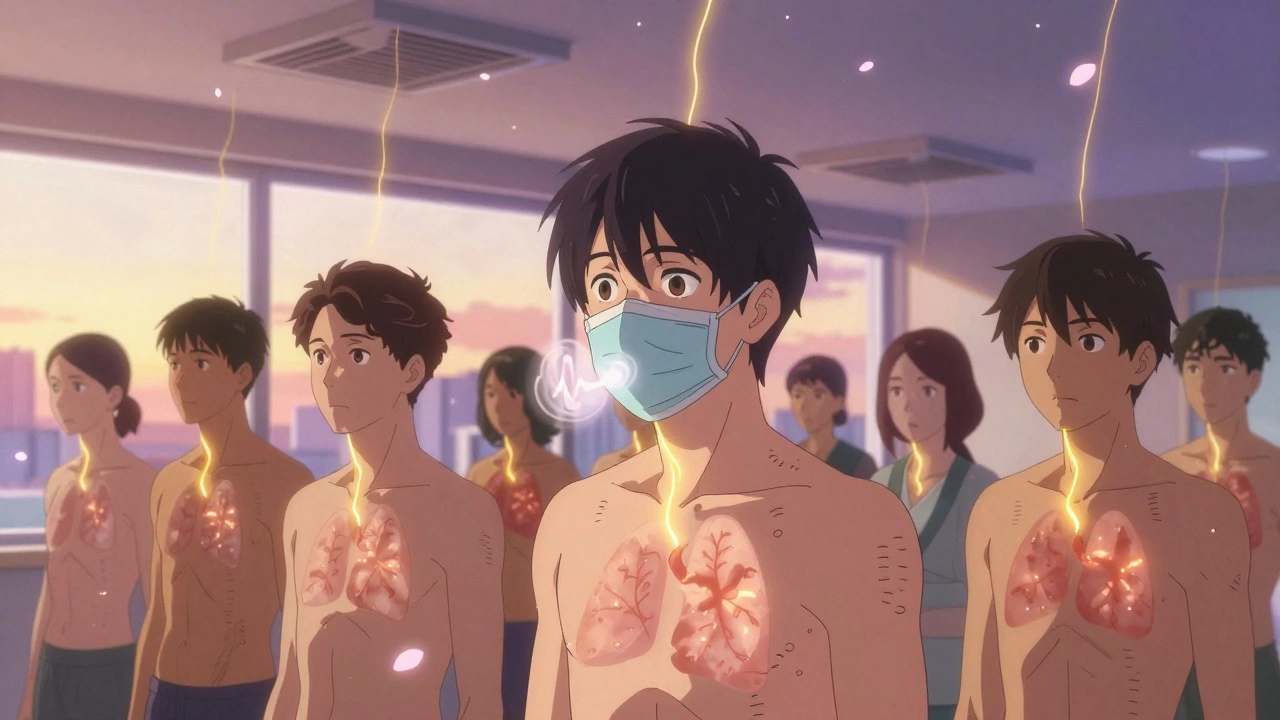
What Exactly Is Drug-Induced Pulmonary Fibrosis?
Pulmonary fibrosis means scar tissue builds up in your lungs. Think of it like rust inside your air sacs-stiff, thick, and unable to expand. Normally, your lungs breathe in oxygen and pass it into your blood. When fibrosis sets in, that exchange slows down. You start gasping for air during simple tasks: walking to the mailbox, climbing stairs, even talking.
Drug-induced pulmonary fibrosis (DIPF) happens when certain medications trigger this scarring. It’s not an allergic reaction. It’s not overdosing. It’s unpredictable. One person takes the same pill for years with no issue. Another develops lung damage after just a few months. No one knows why. The Pulmonary Fibrosis Foundation says it best: “It is not known why some people who use these drugs develop pulmonary fibrosis, while most do not.”
The damage starts small-tiny inflammation in the lung walls. Over time, your body tries to heal itself by laying down collagen, the same material that makes up scar tissue. But in the lungs, that scar doesn’t go away. It piles up. And once it’s there, it’s hard to undo.
The Top Medications That Cause Lung Scarring
There are over 50 drugs linked to this condition. But a handful stand out because they’re so commonly prescribed-and their risks are so often overlooked.
- Nitrofurantoin: Used for urinary tract infections, especially in older women. It’s cheap, effective, and often taken for months as a preventive. But after 6 months to 10 years, some people start coughing. By the time they see a doctor, the lung damage is already advanced. In New Zealand, it was the #1 drug linked to lung scarring between 2014 and 2024, with 47 reported cases.
- Methotrexate: A staple for rheumatoid arthritis and psoriasis. It works by calming the immune system. But in 1-7% of users, it triggers acute lung inflammation that can turn into permanent scarring. In New Zealand, 45 cases were reported in the same time period. The symptoms? Dry cough, fever, fatigue-often mistaken for a cold or flu.
- Amiodarone: A heart rhythm drug. People take it for years after a heart attack or arrhythmia. But after 6-12 months, and especially after taking more than 400 grams total, it can cause irreversible lung damage. About 5-7% of long-term users develop fibrosis. The scary part? It can keep getting worse even after you stop taking it.
- Bleomycin: A chemotherapy drug. Used for testicular cancer and lymphoma. Up to 20% of patients get lung toxicity. The risk spikes with higher doses and older age. Unlike other drugs, bleomycin can cause rapid, life-threatening lung injury within weeks.
- Cyclophosphamide: Another chemo agent. About 3-5% of users develop lung scarring. It’s often used with other drugs, making it harder to spot which one is to blame.
- Immune checkpoint inhibitors: Newer cancer drugs like pembrolizumab and nivolumab. They’ve revolutionized cancer treatment-but in 3-5% of cases, they turn the immune system against the lungs, causing severe inflammation and fibrosis. These cases are rising fast.
And these aren’t rare outliers. Between January 2014 and September 2024, New Zealand’s pharmacovigilance system recorded 173 cases of drug-related lung scarring. Thirty of those patients died. That’s a 17.3% death rate. And that’s just one country.
Why Is It So Hard to Diagnose?
Doctors don’t always look for drug-induced lung damage. Why? Because it doesn’t look like anything else.
There’s no single X-ray pattern. No blood test. No biomarker that says, “This is methotrexate doing this.” The symptoms-dry cough, shortness of breath, fatigue-are the same as asthma, pneumonia, or just getting older. Many patients are told they’re “just out of shape” or “getting old.” One Reddit user wrote: “I was told my cough was from allergies for 8 weeks. By the time I got a CT scan, I’d lost 30% of my lung function.”
Diagnosis requires a detective’s work. Your doctor needs to know every pill you’ve taken in the last year-even supplements and antibiotics you took once. They need to rule out infections, autoimmune diseases, and environmental exposures like asbestos or silica. If you’re on one of the high-risk drugs and you’re having trouble breathing, the first question should be: Could this be the medication?
What Happens If You Keep Taking the Drug?
Stopping the drug is the single most important step. In fact, it’s the only thing that can stop the damage.
Studies show that 89% of patients improve within 3 months after quitting the offending drug. But if you keep taking it? The scarring keeps growing. And once the lungs are badly scarred, they don’t heal. Up to 25% of patients end up with permanent lung damage-even after stopping the drug.
Amiodarone is especially dangerous here. Because it sticks around in your body for months, the lung damage can keep progressing even after you stop taking it. That’s why early detection matters so much.
And yes, some people die from it. The mortality rate for severe cases of amiodarone-induced fibrosis is 10-20%. For methotrexate pneumonitis, it’s even higher if not caught fast.
How Is It Treated?
There’s no magic pill to reverse fibrosis. But there are steps that can help.
- Stop the drug immediately. This isn’t optional. Delaying by weeks can cost you lung function.
- Corticosteroids. High-dose prednisone (0.5-1 mg per kg of body weight) is often used for 3-6 months to calm inflammation. It doesn’t fix the scar, but it can stop it from getting worse.
- Oxygen therapy. If your blood oxygen drops below 88%, you’ll need supplemental oxygen. This isn’t just comfort-it’s survival.
- Pulmonary rehab. Breathing exercises and physical therapy can help you stay active and improve quality of life-even with reduced lung capacity.
Some patients need lung transplants. But that’s a last resort. Transplants come with their own risks-and you have to be healthy enough to qualify. Most people who get them are under 65 and still have decent heart and kidney function.

Who’s at Risk?
You might think only the elderly or the very sick are at risk. But that’s not true.
Older adults are more likely to develop fibrosis, especially from nitrofurantoin and amiodarone. But younger people on methotrexate or immunotherapy are also vulnerable. Women are more often affected by nitrofurantoin, likely because they’re prescribed it more for UTIs. Men on amiodarone for heart conditions are at higher risk for long-term damage.
Smokers? Higher risk. People with pre-existing lung conditions? Higher risk. People taking multiple drugs? Higher risk. And if you’ve had lung damage from one drug before? You’re more likely to get it again from another.
What Can You Do to Protect Yourself?
You can’t avoid all medications. But you can protect yourself.
- Ask your doctor: “Could this medication cause lung problems?” Don’t be shy. If they look confused, ask for a written list of side effects.
- Know the warning signs: A dry cough that won’t go away. Breathlessness during normal activities. Unexplained fatigue. Fever without infection. These aren’t normal aging signs. They’re red flags.
- Get tested if you’re on high-risk drugs: If you’re taking methotrexate, amiodarone, or nitrofurantoin long-term, ask for a baseline pulmonary function test. Repeat it every 6-12 months. It’s a simple breathing test. Takes 10 minutes. Could save your life.
- Track your meds: Keep a list of every pill you take, including doses and start dates. Bring it to every appointment.
- Don’t ignore symptoms: If you’re on one of these drugs and you start coughing or struggling to breathe, don’t wait. Go to the doctor. Say: “I’m on [drug name]. Could this be lung damage?”
The Pulmonary Fibrosis Foundation launched a new education program for primary care doctors in 2024. Early results? A 32% drop in diagnostic delays. That’s progress. But it’s not enough. Most doctors still don’t screen.
The Bigger Picture
Drug-induced pulmonary fibrosis isn’t going away. In fact, it’s getting worse. Over the past decade, reported cases have risen by 23.7%. Why? More drugs. More people on long-term meds. More cancer immunotherapies. More elderly patients with multiple conditions.
Pharmaceutical companies are developing powerful new drugs every year. But safety testing for lung toxicity? It’s still weak. Most trials last 6-12 months. Fibrosis can take years to show up. So we’re playing catch-up.
The good news? We’re starting to pay attention. New Zealand’s health agency issued a public alert in December 2024. The European Respiratory Society now recommends baseline lung tests before starting high-risk drugs. Researchers are hunting for genetic markers that might predict who’s at risk.
But until then, the responsibility falls on you and your doctor. Don’t assume safety. Don’t wait for symptoms to get worse. Ask questions. Get tested. Speak up.
Your lungs can’t tell you they’re being damaged. But you can learn to listen.







Katie Harrison
December 9, 2025 AT 15:06Mona Schmidt
December 11, 2025 AT 02:47Guylaine Lapointe
December 11, 2025 AT 15:40Chris Marel
December 11, 2025 AT 20:28Angela R. Cartes
December 13, 2025 AT 16:46Larry Lieberman
December 14, 2025 AT 22:22Brianna Black
December 15, 2025 AT 10:49Shubham Mathur
December 15, 2025 AT 15:22Stacy Tolbert
December 17, 2025 AT 06:50Lauren Dare
December 19, 2025 AT 06:11