Carbamazepine Dose Adjustment Calculator
Dose Adjustment Calculator
This tool helps determine appropriate carbamazepine dose adjustments during pregnancy based on trimester. Always consult with your healthcare provider before making medication changes.
Your Adjusted Dose
Quick Takeaways
- Carbamazepine crosses the placenta and can raise the risk of certain birth defects, especially neural tube defects.
- Seizure control during pregnancy is critical - stopping the drug abruptly is far riskier than a modest increase in congenital risk.
- Therapeutic drug monitoring (TDM) becomes more important because pregnancy can lower carbamazepine levels.
- Breastfeeding while on carbamazepine is generally considered safe at typical doses, but infant monitoring is advised.
- Alternative medications such as lamotrigine may offer lower teratogenic risk, but each case needs personalized discussion with a neurologist.
When a woman discovers she’s pregnant while taking carbamazepine, the first instinct is panic. carbamazepine pregnancy questions flood the internet, but the answer isn’t a simple yes or no. Below we break down what the drug does, how pregnancy changes its behavior, and which steps can keep both mom and baby as safe as possible.
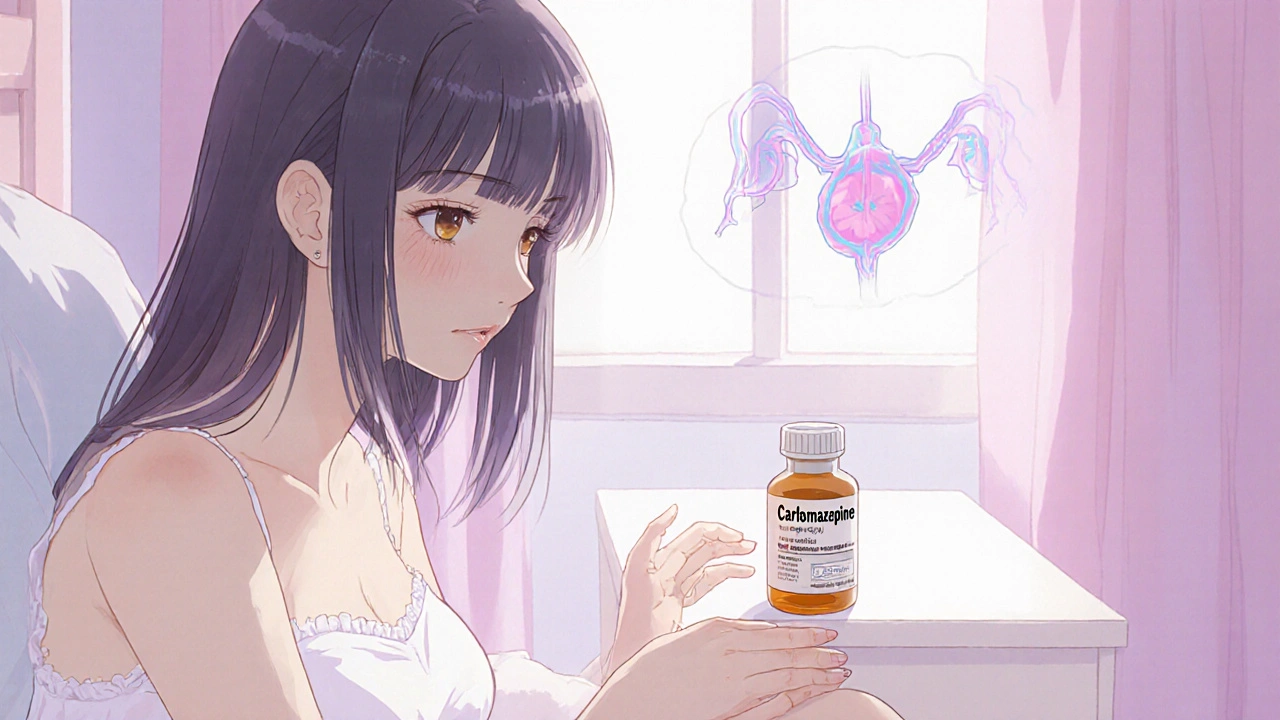
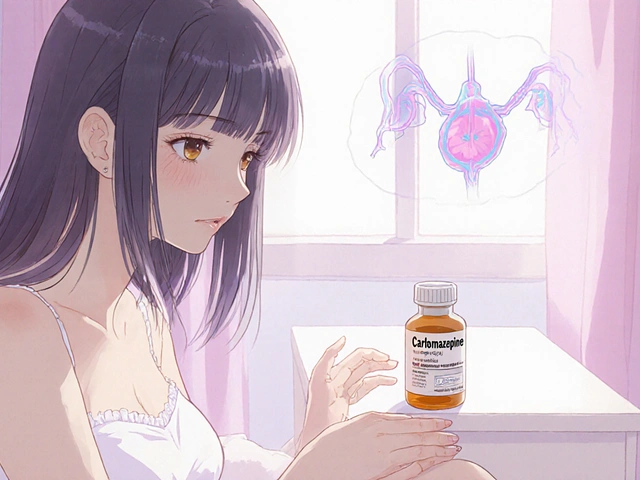
Carbamazepine is an anticonvulsant and mood stabilizer that works by dampening abnormal electrical activity in the brain. It’s most commonly prescribed for epilepsy and bipolar disorder. The drug’s chemical formula is C15H12N2O, and it’s been on the market since the 1960s. While effective, carbamazepine belongs to a class of medications known for crossing the placenta.
Pregnancy is a physiological state that reshapes hormone levels, blood volume, and organ function. These changes can affect how drugs are absorbed, distributed, metabolized, and eliminated-a concept called pharmacokinetic alteration. For carbamazepine, the key alteration is a faster clearance, meaning blood levels often drop as the pregnancy progresses.
Why Seizure Control Matters More Than Ever
Uncontrolled seizures pose a direct threat to both mother and fetus. A convulsion can lead to falls, hypoxia, or even premature labor. Therefore, the consensus among neurologists is to keep a stable, therapeutic level of carbamazepine throughout pregnancy rather than stopping it abruptly.
In practice, most clinicians recommend increasing the dose by 30‑50 % once the second trimester begins, then fine‑tuning based on regular blood tests. This approach balances seizure control with the known teratogenic risks.
Understanding Teratogenic Risk
Teratogenicity refers to a drug’s ability to cause developmental abnormalities in a fetus. For carbamazepine, the most documented malformations are neural tube defects (NTDs) such as spina bifida, as well as craniofacial anomalies, cardiac defects, and fingernail hypoplasia.
Large registry studies estimate the overall risk of major congenital malformations at about 4‑6 % for carbamazepine‑exposed pregnancies, compared with a baseline of 2‑3 % in the general population. The specific risk for NTDs hovers around 1 %, roughly double the background rate.
How Pregnancy Changes Carbamazepine Levels
During pregnancy, estrogen induces hepatic enzymes-especially CYP3A4-that accelerate carbamazepine metabolism. The result is a drop in trough concentrations that can be up to 40 % lower by the third trimester.
Because of this, therapeutic drug monitoring (TDM) becomes essential. Therapeutic drug monitoring involves measuring carbamazepine plasma levels every 4‑6 weeks and adjusting the dose to keep concentrations within the target range of 4-12 µg/mL. Consistent monitoring helps avoid breakthrough seizures while limiting the dose increase to the lowest effective amount.
Alternative Medications: Is Lamotrigine Safer?
When a patient is newly diagnosed or can safely switch, many doctors consider lamotrigine. Lamotrigine is another anticonvulsant with a lower reported teratogenic profile, especially regarding neural tube defects. However, lamotrigine also undergoes rapid clearance in pregnancy, often requiring dose escalations of up to 400 %.
Below is a quick comparison of the two drugs during pregnancy:
| Attribute | Carbamazepine | Lamotrigine |
|---|---|---|
| Major malformation risk | 4‑6 % | 2‑3 % |
| Neural tube defect rate | ~1 % | ~0.3 % |
| Placental transfer | High | Moderate |
| Typical dose increase in 2nd/3rd trimester | 30‑50 % | 200‑400 % |
| Evidence for seizure control | Strong for focal seizures & bipolar | Effective, especially for generalized seizures |
Guidelines from Regulatory Bodies
The FDA classifies carbamazepine as Pregnancy Category D, indicating positive evidence of risk but also that the potential benefits may outweigh the risks for serious conditions. In contrast, lamotrigine is Category C.
Guidelines from the American Academy of Neurology (AAN) and the International League Against Epilepsy (ILAE) stress individualized risk assessment, thorough counseling, and close monitoring rather than a blanket discontinuation.
Practical Steps for Expectant Mothers on Carbamazepine
- Notify your healthcare team early. Your neurologist, obstetrician, and primary care provider should coordinate care from the first trimester.
- Schedule Therapeutic drug monitoring every 4‑6 weeks. Bring the latest lab results to each appointment.
- Discuss folic acid supplementation. A daily 4 mg dose (high‑dose) is recommended for women on carbamazepine, as it may lower NTD risk.
- Ask about genetic counseling. While most carbamazepine‑related malformations are sporadic, a counselor can clarify personal risk factors.
- Monitor for side effects such as drowsiness, rash, or signs of blood dyscrasias. Report any new symptoms promptly.
- If you’re considering switching to lamotrigine, do it well before trying to conceive to allow a stable dosage and monitoring period.
- For breastfeeding, keep the infant’s serum carbamazepine level under observation. Most studies find infant exposure ≤1 % of maternal levels, which is generally safe.

What About Breastfeeding?
Carbamazepine is excreted into breast milk at low levels. The American Academy of Pediatrics considers it compatible with breastfeeding, especially when the mother’s dose is ≤600 mg/day. Still, pediatricians often recommend checking the baby’s weight gain and looking out for excessive sedation.
Common Myths Debunked
- Myth: “If I stop carbamazepine, my baby will be completely safe.”
Fact: Stopping the drug can trigger severe seizures, which are far more dangerous than the modest increase in birth defect risk. - Myth: “All antiepileptic drugs are equally risky.”
Fact: Teratogenic potential varies widely; lamotrigine and levetiracetam are generally considered lower‑risk options. - Myth: “Folic acid completely eliminates the risk.”
Fact: High‑dose folic acid reduces NTD incidence but does not erase other possible malformations.
When to Seek Specialist Care
If you experience any of the following, schedule a rapid follow‑up:
- New or worsening seizure activity.
- Rash, fever, or signs of blood disorders (e.g., bruising, fatigue).
- Ultrasound findings that suggest fetal anomalies.
- Difficulty maintaining therapeutic carbamazepine levels despite dose adjustments.
Bottom Line
Carbamazepine can be continued safely during pregnancy when managed with a proactive, collaborative care plan. The key is regular monitoring, appropriate dose adjustments, high‑dose folic acid, and open communication with your medical team.
Can I stop carbamazepine as soon as I find out I'm pregnant?
Stopping abruptly raises the risk of severe seizures, which can harm both you and the baby. Most experts advise continuing the medication with dose adjustments and close monitoring.
What dose of folic acid should I take?
A high‑dose 4 mg folic acid supplement daily is recommended for women on carbamazepine, starting before conception and continuing through the first trimester.
Is breastfeeding safe while on carbamazepine?
Yes, in most cases. The drug passes into milk at low levels, but your pediatrician should monitor the infant for sedation or poor weight gain.
How often should I have blood tests?
Every 4‑6 weeks during pregnancy, or more often if you notice seizure changes or dose adjustments.
Should I consider switching to lamotrigine?
If you’re early in pregnancy or planning to conceive, discuss with your neurologist. Lamotrigine has a lower teratogenic profile but may need larger dose increases as pregnancy progresses.





Joe Waldron
October 22, 2025 AT 17:15Carbamazepine does cross the placenta-yes, the drug reaches the fetus, and that fact alone necessitates vigilant monitoring; seizure control, however, remains paramount, because uncontrolled seizures can be far more catastrophic than a modest increase in congenital‑defect risk; therefore, clinicians typically aim for a therapeutic plasma level throughout pregnancy, adjusting the dose as metabolism accelerates; regular therapeutic drug monitoring every 4–6 weeks, combined with high‑dose folic acid (4 mg daily), can mitigate neural‑tube‑defect risk; remember also to coordinate care among neurologist, obstetrician, and primary‑care provider to fine‑tune dosing, especially during the second and third trimesters.
Tim Blümel
October 29, 2025 AT 14:55Exactly! 🌟 The balance between seizure freedom and teratogenic risk is a tightrope, but with a solid team and consistent blood‑level checks, many moms navigate it safely. Keep the conversation open with your doc, and don’t forget that staying calm really helps both you and the baby! 😊
Joanne Ponnappa
November 5, 2025 AT 13:35Very helpful info-thanks for breaking it down so clearly. 👍 It’s good to know that staying on the medication with proper monitoring is usually safer than stopping completely.
Michael Vandiver
November 12, 2025 AT 12:15Totally agree! Keep those labs coming and the doc in the loop – it makes all the difference 😄
Sajeev Menon
November 19, 2025 AT 10:55Carbamazepine has been a cornerstone therapy for focal seizures and bipolar disorder for decades, and its pharmacokinetic profile during pregnancy is uniquely challenging; as estrogen levels rise, hepatic enzymes such as CYP3A4 are induced, leading to a 30‑50 % increase in drug clearance by the third trimester. This means that a dose that was once therapeutic can suddenly become sub‑therapeutic, putting both mother and baby at risk for breakthrough seizures. Therapeutic drug monitoring (TDM) every 4‑6 weeks is therefore not just a recommendation but a necessity; without regular trough level checks, clinicians are essentially flying blind. In practice, many neurologists start a modest dose increase-often 30 %-once the second trimester is confirmed, then fine‑tune based on the measured plasma concentrations. It’s also crucial to supplement with high‑dose folic acid (4 mg daily) from preconception through at least the first twelve weeks, as this has been shown to reduce the incidence of neural‑tube defects, though it does not eliminate other malformations. While the overall major‑malformation risk for carbamazepine hovers around 4‑6 %, the baseline risk in the general population is 2‑3 %, so the absolute increase is modest, but still meaningful. Another factor to consider is the drug’s placental transfer rate, which is high, meaning fetal exposure mirrors maternal plasma levels fairly closely. If a seizure does occur, the maternal hypoxia or trauma from a fall can be far more harmful than the teratogenic risk, reinforcing why abrupt discontinuation is contraindicated. Some patients choose to switch to lamotrigine before conception; lamotrigine carries a lower reported teratogenic risk but often requires dose escalations of up to 400 % during pregnancy due to similar metabolic induction. This switch should be done well before trying to conceive, allowing time for stabilization and dose‑finding. Breastfeeding while on carbamazepine is generally considered safe, as drug levels in breast milk are low-typically less than 1 % of maternal serum levels-but infant monitoring for sedation or poor weight gain remains prudent. Finally, open communication among the patient, neurologist, and obstetrician cannot be overstated; coordinated care ensures that dose adjustments are made promptly, side‑effects are caught early, and the mother feels supported throughout the pregnancy journey.
Rachael Turner
November 26, 2025 AT 09:35It’s all about that teamwork, staying on top of labs, and not letting fear drive sudden changes – the safest path is a steady, monitored approach.
Suryadevan Vasu
December 3, 2025 AT 08:15Consistent monitoring and dose adjustment keep both mother and baby safe.
Vin Alls
December 10, 2025 AT 06:55Spot on! Think of it as a delicate choreography-each lab result is a step, each dose tweak a graceful pirouette, and together they create a safe, harmonious performance for both mom and child.
Tiffany Davis
December 17, 2025 AT 05:35I appreciate the balanced view; staying informed and working closely with healthcare providers is clearly the best strategy.
Don Goodman-Wilson
December 24, 2025 AT 04:15Oh sure, “just keep taking that risky drug” while we ignore the obvious fact that pharma pushes dangerous meds on us-real eye‑opener.
Bret Toadabush
December 31, 2025 AT 02:55They don't want you to know that the big pharmas hide the real stats-who really decides what's safe?
Diane Thurman
January 7, 2026 AT 01:35Honestly, this is basic med info-anyone can read the label, no need for all the drama.
Iris Joy
January 14, 2026 AT 00:15Remember you’re not alone in this-lean on your care team, keep those appointments, and trust that with careful monitoring you can protect both your health and your baby’s future.