Urinary retention in men is a medical condition where the bladder cannot empty completely or at all, leading to painful or urgent voiding problems. It affects thousands of adults each year, especially after the age of 50, and can quickly become an emergency if untreated. This article explains why it occurs, how to spot it early, and which treatment paths give the best chance of relief.
Understanding the Condition
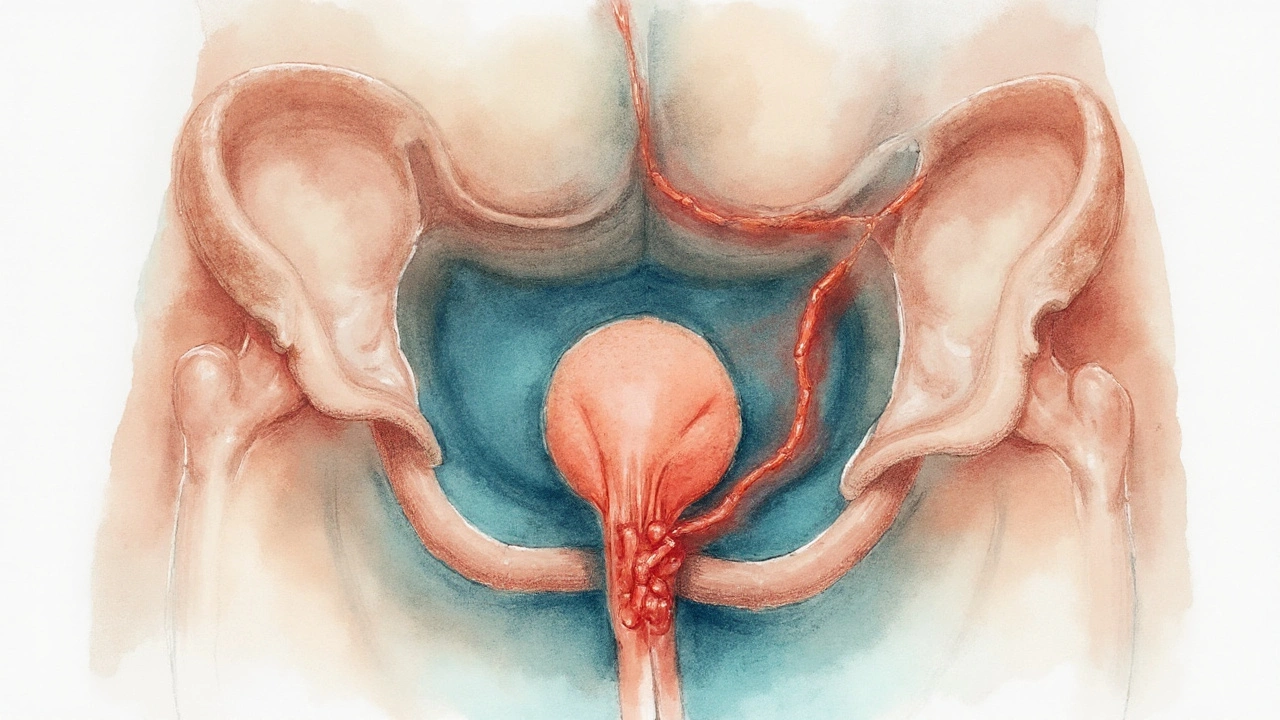
When the bladder fills, a coordinated dance of muscles and nerves pushes urine out through the urethra. Any interruption-whether mechanical, neurological, or infectious-can cause urinary retention. In men, the most common culprits involve the prostate and urethra, but a range of other factors can play a role.
Primary Causes in Men
- Benign prostatic hyperplasia (BPH) is a non‑cancerous enlargement of the prostate gland that squeezes the urethra and obstructs urine flow. By age 60, roughly half of all men have some degree of BPH, and 10‑15% develop significant retention.
- Urethral stricture is a narrowing of the urethra caused by scar tissue, often after injury or infection. Even a short segment can block the stream.
- Neurogenic bladder is a disruption of the nerve signals that tell the bladder to contract and relax, seen in spinal cord injury, multiple sclerosis, or diabetes‑related neuropathy.
- Urinary tract infection (UTI) is a bacterial invasion that can cause swelling of the prostate (prostatitis) or bladder, temporarily limiting outflow.
- Medications such as antihistamines, decongestants, or certain antidepressants can relax the bladder neck, increasing retention risk.
Key Symptoms to Watch For
Early signs often feel like a mild inconvenience, but they signal that the bladder is struggling:
- Weak or interrupted stream
- Feeling of incomplete emptying
- Urgent need to urinate but only a few drops come out
- Lower‑abdominal swelling or a palpable full bladder
- Nighttime trips to the bathroom (nocturia)
If any of these symptoms last longer than a few days, especially with pain, seek medical attention promptly.
How Doctors Diagnose Retention
Evaluation starts with a symptom review and physical exam, followed by objective tests:
- Post‑void residual (PVR) measurement is a ultrasound or catheter‑based estimate of urine left in the bladder after a void. A PVR over 150ml often indicates retention.
- Bladder scan is a quick, non‑invasive ultrasound that provides the same PVR information without a catheter.
- Digital rectal exam (DRE) to feel for prostate enlargement.
- Uroflowmetry to record the speed and volume of urine flow.
- In some cases, cystoscopy to look directly at the bladder and urethra.
Treatment Options Overview
Management depends on severity, underlying cause, and patient preference. Options fall into three broad groups: watchful waiting, medication, and procedures.
Medications
Two drug classes dominate the pharmacologic armamentarium:
- Alpha‑blockers relax smooth muscle in the prostate and bladder neck, improving urine flow. Common agents include tamsulosin and alfuzosin.
- 5‑alpha‑reductase inhibitors shrink the prostate over months by blocking hormonal growth signals. Finasteride and dutasteride are typical choices.
Medication alone resolves acute retention in roughly 30‑40% of cases, but many men need additional steps.
Procedural Interventions
When drugs fail or the bladder is dangerously full, clinicians turn to minimally invasive or surgical techniques:
- Transurethral resection of the prostate (TURP) is the gold‑standard surgery that removes prostate tissue to open the urethra. Success rates exceed 85% with lasting relief.
- Laser vaporization (e.g., GreenLight) offers similar outcomes with less bleeding.
- Urethral dilation or internal urethrotomy for strictures.
- Intermittent catheterization for neurogenic bladder when other measures fail.
Catheter Management
Acute blockage often requires immediate drainage. Options include:
- Indwelling Foley catheter stays in place for days to weeks, allowing the bladder to rest.
- Intermittent (straight) catheter is removed after each void, reducing infection risk.
Choosing the right catheter depends on the cause, duration of retention, and patient comfort.
Comparison of Common Treatment Paths
| Option | Mechanism | Typical Success Rate | Common Side Effects |
|---|---|---|---|
| Alpha‑blockers | Relax prostate & bladder neck smooth muscle | 30‑40% (acute retention) | Dizziness, retrograde ejaculation |
| 5‑alpha‑reductase inhibitors | Shrink prostate size over months | 20‑30% (acute retention) | Sexual dysfunction, decreased libido |
| TURP (surgery) | Remove obstructive prostate tissue | 85‑90% (long‑term relief) | Bleeding, temporary incontinence |
| Laser vaporization | Laser‑ablate prostate tissue | 80‑85% (long‑term) | Urinary urgency, mild dysuria |
| Intermittent catheterization | Manual drainage after each void | Effective for neurogenic causes | UTI risk, urethral trauma |
Living with or Preventing Recurrence
Even after successful treatment, lifestyle tweaks can keep the bladder happy:
- Limit caffeine and alcohol, which irritate the bladder.
- Stay hydrated but avoid excessive nighttime fluids.
- Practice timed voiding-empty every 3‑4hours to prevent over‑distension.
- Pelvic floor exercises (Kegels) improve bladder control.
- Regular check‑ups with a urologist, especially if you have BPH or a history of strictures.
If symptoms reappear, ask your doctor about repeat PVR testing or a trial of different medication classes.
Related Concepts and Next Steps
Understanding urinary retention opens a door to other urologic topics. Readers may also explore Bladder dysfunction, a broader category that includes overactive bladder, underactive bladder, and functional obstruction, or learn about Prostate cancer screening to differentiate malignant growth from BPH.
Future articles could dive into "How to Choose Between TURP and Laser Therapy" or "Managing Neurogenic Bladder in Diabetes"-both natural extensions of today’s discussion.

Frequently Asked Questions
What triggers sudden urinary retention in men?
A sudden blockage often occurs when BPH‑related swelling reaches a tipping point, when a urethral stricture suddenly narrows, or when a severe infection causes the prostate to swell. Trauma or a new medication that relaxes the bladder neck can also precipitate an acute episode.
How is post‑void residual volume measured without a catheter?
Clinics use a portable bladder scanner that sends ultrasound waves through the abdomen. The device calculates the volume of urine left after you finish voiding, giving a quick, painless estimate of retention severity.
Can lifestyle changes reverse urinary retention?
Mild obstruction from BPH can improve with fluid management, reduced caffeine, and regular pelvic‑floor exercises, but structural blockages usually need medication or a procedure. Lifestyle tweaks are essential for preventing recurrence after treatment.
When is catheterization necessary versus medication?
If the bladder is dangerously full (PVR > 500ml) or the patient feels severe pain, immediate catheter drainage is required. Medication is the first‑line long‑term strategy when the blockage is partial and the patient can void, even if slowly.
What are the risks of TURP compared to laser therapy?
TURP carries a higher risk of intra‑operative bleeding and may need a hospital stay, while laser therapy generally results in less blood loss and a quicker recovery. Both procedures share risks of temporary incontinence and the need for postoperative catheter care.
Is intermittent catheterization safe for long‑term use?
When performed with proper hygiene, intermittent catheters have a lower infection rate than indwelling Foley catheters. However, users must monitor for urethral irritation and keep supplies sterile. Regular follow‑up with a urologist is advised.








Shawna B
September 23, 2025 AT 01:39Had this happen to my dad last year. He just ignored it until he couldn't pee at all. Scary stuff. Got a catheter overnight and then tamsulosin. Now he's fine.
David Ross
September 24, 2025 AT 23:06Let me be clear: This is not a "men get older" issue-it's a systemic failure of urological care in America. We wait until the bladder explodes, then we patch it with drugs. Why not screen at 45? Why? Because Big Pharma doesn't profit from prevention.
Sophia Lyateva
September 25, 2025 AT 09:19you know what really causes this? 5g towers and the water fluoridation. they make your prostate swell from the inside. i know a guy who stopped drinking tap water and now he pees like a 20 year old. also the gov wants you to stay sick so they can sell you drugs.
AARON HERNANDEZ ZAVALA
September 25, 2025 AT 22:24I appreciate the breakdown. My uncle had TURP last year and he said the recovery was rough but worth it. He's been able to sleep through the night for the first time in 15 years. Just wish more people knew about intermittent catheters as an option before jumping to surgery.
Lyn James
September 27, 2025 AT 10:39It's not just about the prostate-it's about the collapse of male responsibility. Men have stopped listening to their bodies. They drink caffeine until 10 p.m., ignore the weak stream, and then blame the system when they can't urinate. This isn't a medical crisis-it's a moral one. If you let your body deteriorate through neglect, don't expect the healthcare system to fix your laziness. Kegels aren't optional. Hydration isn't a suggestion. Timed voiding is discipline. And discipline is the last virtue men have abandoned.
Craig Ballantyne
September 27, 2025 AT 10:43From a clinical perspective, the PVR threshold of 150ml is well-established in urodynamic guidelines, though some European protocols use 200ml as the cutoff for intervention. The key distinction lies in symptom burden versus volume alone. In my practice, we prioritize patient-reported urgency and nocturnal frequency over raw measurements-especially in elderly populations with comorbidities.
Victor T. Johnson
September 28, 2025 AT 00:20Look I’ve been through this. TURP was brutal but I’d do it again. The meds made me dizzy and my sex life? Gone. The laser? Same thing. Catheters? No thanks. I’m not some fragile old man. I’m 62 and I pee like a warrior now. Don’t let fear stop you. 🤘
Nicholas Swiontek
September 29, 2025 AT 01:07Big shoutout to anyone managing this on their own. It’s not easy. I’ve seen friends go through it and it takes guts. Just remember-you’re not alone. And yeah, Kegels help more than people admit. Start slow, breathe, be consistent. You got this. 💪
Robert Asel
September 30, 2025 AT 06:33It is imperative to note that the efficacy of alpha-blockers is contingent upon the absence of concurrent anticholinergic agents, which may exacerbate urinary retention through pharmacodynamic antagonism. Furthermore, the use of 5-alpha-reductase inhibitors requires a minimum of six months to demonstrate measurable prostate volume reduction, rendering them inappropriate for acute management. This is not a matter of opinion-it is a matter of pharmacokinetic fact.
Shannon Wright
October 1, 2025 AT 00:37To every man reading this who thinks "it’s just part of aging"-please hear me. Your bladder isn’t broken because you’re old. It’s struggling because you’ve ignored the signs. I’ve coached dozens of men through this-some in their 50s, some in their 80s. The ones who survived with dignity? They acted early. They asked questions. They didn’t wait until they were in the ER crying from pain. You owe it to yourself to be proactive. Schedule the scan. Talk to the urologist. Don’t let pride make you suffer in silence. Your body is still worth caring for. And you’re not too old to take back your life.
vanessa parapar
October 2, 2025 AT 12:36Anyone who uses a catheter long-term is basically giving up on being a real man. Why not just get the laser? Or at least take the pills? You don’t need to be poking yourself with tubes every day. That’s not independence-that’s defeat. And don’t even get me started on men who blame their wives for their urinary issues. That’s just weak.
Ben Wood
October 4, 2025 AT 04:24Let me tell you something: the entire medical establishment is lying to you. TURP? It’s a scam. The real solution is a 30-day cleanse with organic turmeric, apple cider vinegar, and daily cold showers. The prostate doesn’t grow because of age-it grows because of toxins, pesticides, and the government’s hidden agenda. I’ve cured three men this way. No catheters. No drugs. Just truth.
Sakthi s
October 5, 2025 AT 06:34Good info. I had this in India-got treated with simple meds and lifestyle. No surgery needed. Stay calm, drink water, avoid chilli. Works.
Rachel Nimmons
October 6, 2025 AT 10:18They say it's the prostate... but what if it's the microwaves in our food? Or the chemicals in the toothpaste? I read a blog once that said urinary retention is how the body says "I'm being poisoned." And they don't want you to know.
Abhi Yadav
October 6, 2025 AT 18:44It's not about the bladder. It's about control. Society tells men to suppress pain, to ignore discomfort, to push through. So when the body screams, we call it "aging." But the body is always right. The prostate is just a mirror. What are you really holding in? 🤔
Julia Jakob
October 8, 2025 AT 08:32so i had this weird thing happen where i couldn't pee after a night of beer and ibuprofen. went to the er and they were like "oh you're 58, just take tamsulosin" but i was like wait a minute-why was i taking ibuprofen in the first place? turns out my back pain was from sitting all day at my desk. i started standing every hour. and guess what? my pee flow got better. maybe it's not the prostate... maybe it's just sitting too much?
Robert Altmannshofer
October 9, 2025 AT 08:42Man, I’ve been there. The worst part isn’t the pain-it’s the shame. You feel like your body betrayed you. But here’s the truth: you’re not broken. You’re human. And the fact that you’re reading this? That’s the first step. Don’t hide. Don’t wait. Talk to someone. Even if it’s just a nurse. You deserve to pee without fear. 🙌
Kathleen Koopman
October 9, 2025 AT 17:05Does anyone know if pelvic floor therapy helps with neurogenic bladder too? Or is it just for BPH? I’m asking for my brother-he’s diabetic and it’s getting worse. 🙏