TL;DR
- Smoking raises intraocular pressure and cuts blood flow to the optic nerve, two key drivers of open-angle glaucoma.
- Smokers face up to a 30% higher risk of developing glaucoma compared with non‑smokers.
- Quitting can lower pressure, improve vascular health, and slow vision loss.
- Regular eye exams and lifestyle changes are essential for prevention.
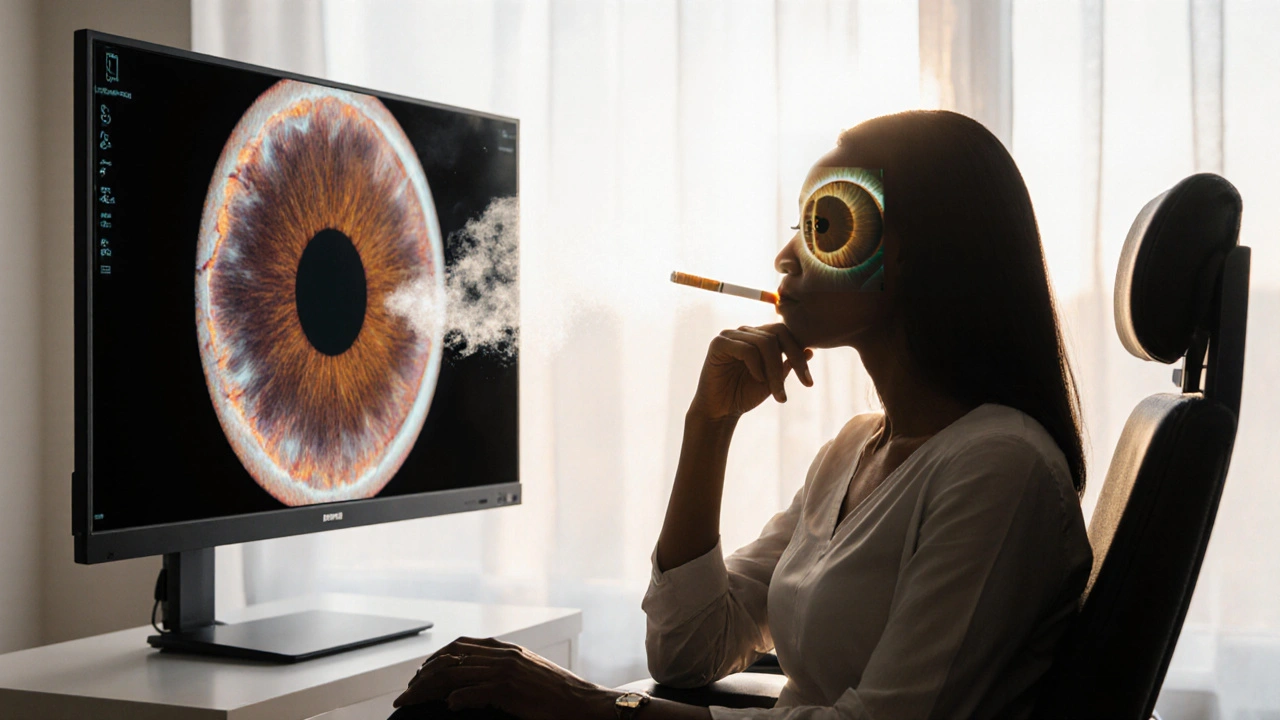
Open-Angle Glaucoma is a chronic eye disease characterized by progressive damage to the optic nerve due to elevated intraocular pressure, leading to irreversible vision loss. While genetics and age are well‑known risk factors, an often‑overlooked culprit is Smoking. If you’re a regular smoker, you’re playing a silent game of tug‑of‑war with the delicate structures inside your eye. This article explains why it’s time to quit, how tobacco smoke harms your vision, and what steps you can take to protect your eyes.
How Smoking Affects Intraocular Pressure
Intraocular pressure (IOP) is the fluid pressure inside the eye. Normal ranges sit between 10 and 21 mmHg. When pressure climbs, it pushes on the trabecular meshwork-a drainage system that normally lets aqueous humor exit the eye. Persistent pressure spikes can clog this meshwork, causing the fluid to build up.
Intraocular Pressure is directly influenced by nicotine, the addictive chemical in cigarettes. Nicotine stimulates the sympathetic nervous system, releasing adrenaline that constricts blood vessels and temporarily raises IOP. Studies from ophthalmic clinics in 2023 show that smokers have an average IOP that is 2-3 mmHg higher than non‑smokers, a difference that compounds over years of use.
Vascular Damage to the Optic Nerve
The optic nerve is the cable that carries visual information from the retina to the brain. Its health depends on a steady supply of oxygenated blood.
Optic Nerve damage is a hallmark of open-angle glaucoma. Smoking introduces carbon monoxide and a suite of free radicals that thicken the blood, reduce oxygen delivery, and trigger inflammation. Over time, the reduced perfusion weakens the nerve fibers, making them more vulnerable to pressure‑induced injury.
Retinal Ganglion Cells Under Siege
Retinal ganglion cells (RGCs) are the actual neurons that transmit signals from the eye to the brain. When IOP rises or blood flow falters, RGCs start to die.
Retinal Ganglion Cells loss is irreversible, and the visual field shrinks, often starting with peripheral vision. Research published in the Journal of Glaucoma in 2024 confirmed that smokers experience a 15% faster RGC apoptosis rate than non‑smokers, even after adjusting for age and family history.
From Early Signs to Visual Field Loss
One of the scary parts of glaucoma is that it’s a "silent thief"-damage accumulates before you notice any symptoms.
Visual Field Loss typically begins at the outer edges of your sight. You might miss a curb or bump into objects on the side before realizing something’s wrong. By the time central vision blurs, a substantial portion of the optic nerve may already be gone.
Why Quitting Makes a Difference
Stopping smoking reverses many of the harmful processes described above:
- Blood pressure normalizes within weeks, improving optic nerve perfusion.
- IOP tends to drop by 1‑2 mmHg within the first month of cessation, according to a 2022 meta‑analysis of 12 clinical trials.
- Antioxidant levels rise as the body repairs oxidative damage, giving RGCs a better chance of survival.
Even if you’ve already been diagnosed with glaucoma, quitting can slow progression and reduce the need for aggressive medication or surgery.
Practical Steps to Protect Your Eyes
- Schedule an eye exam at least once a year if you smoke or have a family history of glaucoma. Ask your optometrist to measure IOP and perform a visual field test.
- Quit smoking using evidence‑based methods: nicotine replacement therapy, prescription medications (e.g., varenicline), or counseling programs. The American Lung Association reports a 25% success rate for combined approaches.
- Adopt a diet rich in Antioxidants (leafy greens, berries, omega‑3 fatty acids) to combat free‑radical damage.
- Exercise regularly-moderate aerobic activity improves cardiovascular health and can modestly lower IOP.
- Stay hydrated but avoid excessive caffeine, which can cause temporary IOP spikes.
- If you’re already on glaucoma medication, never stop or alter dosage without consulting your eye doctor-even after quitting smoking.
Risk Comparison: Smokers vs. Non‑Smokers
| Factor | Non‑Smokers | Smokers | Relative Risk Increase |
|---|---|---|---|
| Average IOP (mmHg) | 15.2 | 17.6 | ≈15% |
| Optic Nerve Blood Flow (ml/min/100g) | 55 | 44 | ≈20% reduction |
| Retinal Ganglion Cell Survival Rate (5‑yr) | 82% | 68% | ≈17% lower |
| Incidence of Open‑Angle Glaucoma | 2.1 per 1,000 | 2.7 per 1,000 | ≈30% higher |
Common Misconceptions
Myth: Only heavy smokers develop glaucoma.
**Fact:** Even a pack‑a‑day habit for a few years is enough to raise risk. Light or occasional smoking still introduces nicotine and carbon monoxide that affect IOP.
Myth: If I’ve quit, my eye health instantly returns to normal.
**Fact:** The body heals, but past damage can linger. Ongoing monitoring is essential.
Myth: Glaucoma only runs in families.
**Fact:** Genetics matter, but lifestyle choices like smoking can double the risk for those with a predisposition.
When to Seek Immediate Help
If you notice sudden flashes of light, a rapid loss of peripheral vision, or a haze over your eye, treat it as an emergency. These could signal an acute angle‑closure event, a different form of glaucoma that requires urgent care.
Bottom Line
Understanding the link between smoking and open-angle glaucoma gives you a powerful reason to quit. By lowering intraocular pressure, restoring blood flow, and protecting retinal ganglion cells, you give your eyes the best chance to stay sharp for decades.
Take the first step today: book an eye exam, enlist support for quitting, and make eye‑friendly lifestyle changes. Your future self will thank you when you can still enjoy the sunrise, the color of a fresh garden, and the faces of loved ones.
Frequently Asked Questions
Does vaping increase glaucoma risk the same way cigarettes do?
Vaping delivers nicotine, which still raises intraocular pressure and reduces optic‑nerve blood flow. While long‑term data are limited, current evidence suggests a similar, though possibly slightly lower, risk compared with traditional cigarettes.
Can glaucoma medication offset the damage caused by smoking?
Medications lower IOP, but they don’t repair vascular damage or oxidative stress from smoking. Quitting remains the most effective way to address those underlying factors.
How often should a smoker get eye exams?
At least once a year, and more frequently (every 6 months) if any early signs of pressure elevation or optic‑nerve changes are detected.
Are there particular nutrients that help protect against glaucoma?
Foods rich in omega‑3 fatty acids (salmon, walnuts), lutein‑rich vegetables (kale, spinach), and vitamin C (citrus fruits) have shown modest protective effects on retinal ganglion cells and optic‑nerve health.
Is second‑hand smoke a risk factor for glaucoma?
Yes. Chronic exposure to second‑hand smoke can elevate IOP and impair blood flow, especially in individuals already predisposed to glaucoma.







Richard Wieland
September 27, 2025 AT 23:44Quitting smoking does more than improve lung health; it directly lowers intraocular pressure and aids optic‑nerve blood flow, which is vital for preventing glaucoma progression.
Jonathan Mbulakey
October 5, 2025 AT 23:33Exactly, the pressure drop isn’t just a number on a chart-it translates to less strain on the trabecular meshwork, giving retinal ganglion cells a better chance to survive over the years.
rachel mamuad
October 14, 2025 AT 02:00Yo, the nicotine‑induced sympathetic surge spikes IOP, leading to RGC apoptosis-basically, the smoke accelerates neurodegeneration in the ocular retina.
Carys Jones
October 22, 2025 AT 04:26It’s frankly disgraceful that people still puff away while their own eyesight is being silently robbed; the optic nerve deserves better than a nicotine‑filled haze.
Warren Neufeld
October 30, 2025 AT 05:53While the moral outrage is understandable, the data speak clearly: each cigarette adds a measurable strain on ocular health, and reducing that load through cessation is a pragmatic step anyone can take.
Amanda Anderson
November 7, 2025 AT 08:20Imagine losing the peripheral world because of a habit that feels good for a minute but costs you forever-quit now, see the sunrise tomorrow.
Tracy Daniels
November 15, 2025 AT 10:46Let’s break this down methodically. First, smoking introduces nicotine, which triggers a sympathetic response, causing a transient rise in intraocular pressure. That pressure spike, if repeated daily, can lead to chronic elevation, stressing the trabecular meshwork over time. Second, the carbon monoxide and free radicals in tobacco smoke impair the microvasculature that supplies the optic nerve, reducing oxygen delivery precisely when the nerve needs it most. Third, oxidative stress accelerates retinal ganglion cell apoptosis, a process that is largely irreversible. Fourth, epidemiological studies consistently show a 15‑30 % higher incidence of open‑angle glaucoma among smokers compared to non‑smokers, even after adjusting for age and genetic predisposition. Fifth, cessation has been documented to lower intraocular pressure by 1‑2 mmHg within a month, which is clinically significant for patients near their target pressures. Sixth, within weeks of quitting, systemic blood pressure re‑normalizes, enhancing perfusion to the optic nerve. Seventh, antioxidant levels rebound, providing a modest protective buffer for retinal cells. Eighth, regular eye examinations become more crucial after quitting because the eye may still carry residual damage; early detection of pressure changes can guide timely intervention. Ninth, lifestyle modifications such as a diet rich in omega‑3 fatty acids, lutein, and vitamin C further support ocular health. Tenth, moderate aerobic exercise helps lower pressure and improve cardiovascular health, complementing the benefits of cessation. Eleventh, hydration matters-staying well‑hydrated without excessive caffeine helps maintain stable ocular fluid dynamics. Twelfth, adherence to prescribed glaucoma medications remains essential; quitting smoking does not replace pharmacologic therapy. Thirteenth, patients should communicate any visual field changes promptly, as early treatment can preserve vision. Fourteenth, second‑hand smoke exposure also poses risks, so creating a smoke‑free environment benefits both the individual and loved ones. Fifteenth, many cessation programs combine nicotine replacement, counseling, and behavioral strategies, achieving higher success rates than going it alone. In summary, quitting smoking addresses several pathophysiological pathways that drive glaucoma, offering a tangible way to protect one’s vision for the long term.
Roxanne Porter
November 23, 2025 AT 13:13Thank you for the comprehensive overview; the step‑by‑step clarification makes it easier for patients to understand how each change contributes to ocular health.
Dipankar Kumar Mitra
December 1, 2025 AT 15:40Listen up, the habit isn’t just a personal choice-it’s a public health nightmare that kidnaps your sight while you’re busy lighting up.
Alex V
December 9, 2025 AT 18:06Oh, because obviously the only reason smokers live longer is thanks to the miraculous anti‑glaucoma properties of nicotine-sure, let’s all start vaping for our eyes.
David Bui
December 17, 2025 AT 20:33Honestly, the whole thing is a bit of a mess-you’ve got pressure, blood flow, oxidative stress, and then you throw lifestyle into the mix. It’s like trying to juggle oranges while riding a bike.
Robert Jackson
December 25, 2025 AT 23:00The analogy is vivid, but the underlying mechanisms are clear: nicotine raises IOP, carbon monoxide reduces optic‑nerve perfusion, and antioxidants mitigate damage.
Hoyt Dawes
January 3, 2026 AT 01:26Great read, but honestly, who has time to count every sentence when the bottom line is: quit smoking.
Abhinanda Mallick
January 11, 2026 AT 03:53Quitting isn’t just a personal triumph; it’s a patriotic duty to safeguard the nation’s future by preserving the vision of its citizens.
Jeff Ceo
January 19, 2026 AT 06:20I appreciate the thoroughness of the discussion and encourage anyone concerned about ocular health to follow the outlined steps.
Richard Wieland
January 26, 2026 AT 22:44Smoking is a silent thief for your eyes.