For millions of people with type 2 diabetes, the idea of getting off medication isn’t just a dream-it’s a real possibility. Not because the disease vanished, but because the body finally got back some of its balance. This is what experts now call remission-a state where blood sugar stays normal without needing drugs. And the most powerful tool to get there? Losing weight.
What Does Remission Actually Mean?
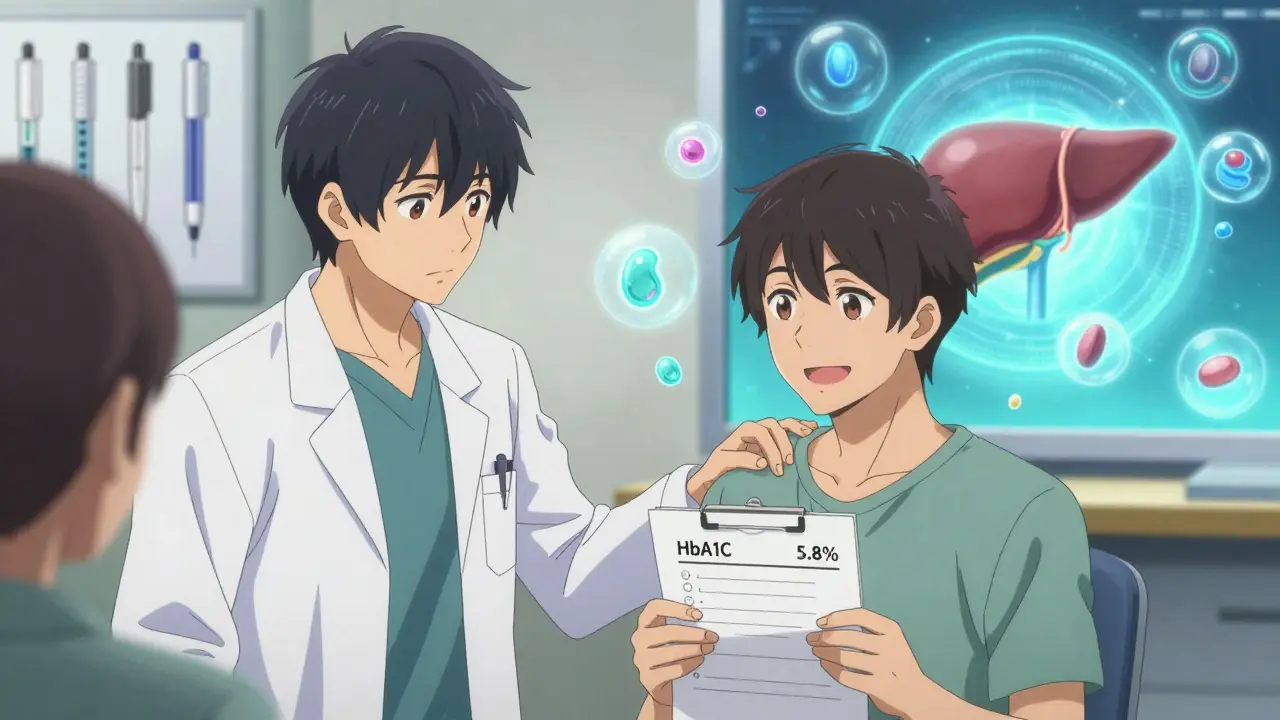
Remission isn’t a cure. It’s not magic. It doesn’t mean your pancreas suddenly healed itself forever. But it does mean your blood sugar has stayed below 6.5% HbA1c for at least three months-without any diabetes medications. That’s the official definition agreed on in 2021 by the American Diabetes Association, the European Association for the Study of Diabetes, Diabetes UK, and the Endocrine Society. Before that, every study used its own rules. Now, doctors have a clear standard.That’s huge. It means if you’ve been on metformin, sulfonylureas, or even insulin, and your HbA1c drops below 48 mmol/mol (6.5%) and stays there for three months after stopping meds, you’re officially in remission. If HbA1c isn’t reliable for you-maybe due to anemia or kidney issues-you can use fasting blood sugar under 126 mg/dL or estimated HbA1c from a continuous glucose monitor instead.
But here’s the catch: if you’re still taking diabetes meds and your HbA1c is low, that’s good control-not remission. The definition was made to be strict on purpose. It’s meant to highlight real change, not just chemical help.
Weight Loss Is the Key Driver
The most consistent factor behind remission? Losing weight. Not a little. Not 5 pounds. At least 10 kilograms (about 22 pounds), and often more.The DiRECT trial, one of the most important studies on this, showed that 46% of people who lost 10kg or more went into remission after one year. Even more telling? After two years, 36% were still in remission. That’s not a fluke. That’s a pattern. And it’s been repeated in other studies-from the UK to Australia.
How does weight loss do this? Fat around the liver and pancreas interferes with insulin production and sensitivity. When you lose that fat, especially from deep inside the belly, your pancreas can start working again. Your liver gets better at managing sugar. Your body stops fighting insulin. It’s like hitting reset on your metabolism.
Studies like DiRECT-Aus proved this works even in diverse populations-not just in wealthy countries or with perfect diets. Total diet replacement programs, where people swap regular meals for nutritionally balanced shakes or soups for a few months, have been especially effective. Then, they slowly reintroduce real food with support.
Who Has the Best Chance?
Not everyone has the same odds. Some people are far more likely to reach remission than others.- Shorter diabetes duration: If you were diagnosed less than five years ago, your chances are much higher. The longer you’ve had high blood sugar, the more damage may have been done to your insulin-producing cells.
- Lower starting HbA1c: Someone with an HbA1c of 7.5% has a better shot than someone at 9.5%. The closer you are to normal, the less your body needs to rebuild.
- No insulin use: People who’ve never needed insulin have the highest success rates. Insulin use often means the pancreas has lost a lot of function.
- Higher weight loss: Losing 15kg or more? Your odds jump even more.
Age doesn’t matter as much as you might think. A 65-year-old who loses 15kg has just as good a shot as a 45-year-old. It’s about the body’s ability to recover, not how many birthdays you’ve had.
What Happens After Remission?
This is where most people get tripped up. Remission doesn’t mean you can go back to old habits. In fact, the biggest risk isn’t failing to lose weight-it’s gaining it back.The DiRECT study showed that remission rates dropped from 46% at one year to 36% at two years. Why? Weight regained. That’s the number one reason blood sugar creeps back up. The body doesn’t forget how to be insulin-resistant. It just needs a little extra fat to flip the switch again.
That’s why experts stress: remission needs maintenance. You still need to eat well, move regularly, and keep seeing your doctor. Annual HbA1c checks are just as important as they were when you were on medication. Your risk for heart disease and nerve damage doesn’t disappear overnight-even if your blood sugar is normal.
Some people stay in remission for years. Others go back after six months. It’s unpredictable. But every year you stay in remission reduces your risk of complications. That’s a win, no matter how long it lasts.
Medication De-Escalation Isn’t the Goal-It’s the Result
Many people think the goal is to stop pills. But that’s backwards. The goal is to get your body working better. Stopping meds is just the side effect.Doctors don’t just pull your meds out of nowhere. They watch your HbA1c closely. They check your weight. They look at your diet and activity. Only when everything is stable for months do they start reducing doses-usually one at a time. Metformin first. Then maybe a GLP-1 agonist. Insulin? That’s the last to go, if at all.
And here’s something many don’t say out loud: you should never stop meds just to chase remission. If your blood sugar is high and you’re at risk for complications, staying on medication is safer than risking damage while trying to lose weight. Remission is a bonus, not a requirement.
Some experts even suggest a second category: medication-supported remission. That’s when someone’s HbA1c is normal, but they still take a low dose of metformin or a GLP-1 drug to help hold it there. That’s not failure. That’s smart management.

What About Surgery?
Bariatric or metabolic surgery isn’t for everyone. But for those who qualify, it’s one of the most effective ways to get into remission. The ARMMS-T2D trial found that 37.5% of people were in remission three years after surgery. That’s higher than diet alone-but it comes with risks. Surgery isn’t a quick fix. It’s a lifelong change.People who get surgery still need to follow strict nutrition plans. They still need to take vitamins. They still need to move. And they still need to be monitored. The body adapts, but it doesn’t forget.
For most people, surgery isn’t the first step. But for those with severe obesity and diabetes that’s hard to control, it’s a powerful option.
The Big Unknowns
We still don’t know everything. Experts admit that.- How long will remission last for most people? No one knows.
- Does being in remission really lower heart attack or stroke risk long-term? We’re still studying it.
- What if your HbA1c stays low but your insulin sensitivity doesn’t improve? Does that count?
- Should the three-month rule be longer? Should the 6.5% threshold be lower?
These aren’t just academic questions. They shape how doctors talk to patients. They affect insurance coverage. They determine who gets access to weight-loss programs.
Right now, the rules are clear enough to guide care-but flexible enough to change as we learn more. As Dr. Roy Taylor said, the current definition isn’t the final answer. It’s a working hypothesis.
What Should You Do?
If you have type 2 diabetes and want to aim for remission:- Work with your doctor to set a realistic weight goal. Start with 5-10% of your body weight.
- Focus on sustainable changes, not quick fixes. A low-calorie diet with protein and fiber works better than extreme diets.
- Get moving. Even 30 minutes of walking most days helps.
- Track your HbA1c and weight regularly.
- Don’t rush to stop meds. Let your doctor guide the process.
- Keep your appointments-even if you feel fine.
Remission isn’t a finish line. It’s a new starting point. One where you’re in charge-not your meds, not your cravings, not your blood sugar numbers. It’s possible. It’s hard. But it’s worth it.
Can type 2 diabetes be cured by losing weight?
No, weight loss doesn’t cure type 2 diabetes. It can lead to remission, which means blood sugar stays normal without medication-but the underlying tendency for insulin resistance remains. If weight is regained, blood sugar can rise again. Remission is a reversal of symptoms, not a cure of the disease.
How much weight do I need to lose to get into remission?
Losing at least 10 kilograms (about 22 pounds) significantly increases your chances. People who lose 15kg or more have even higher success rates. The more weight lost, especially from the liver and pancreas, the better the chance of remission. But even smaller losses can improve blood sugar control.
Can I stop my diabetes meds on my own if my blood sugar improves?
Never stop diabetes medication without your doctor’s guidance. Even if your blood sugar looks better, stopping suddenly can cause dangerous spikes or drops. Your doctor will monitor your HbA1c and weight over time before safely reducing or stopping meds.
Does remission mean I no longer need diabetes checkups?
No. Even in remission, you still need annual HbA1c tests and regular checkups for eye, kidney, and nerve health. The risk of complications doesn’t disappear just because your blood sugar is normal. Ongoing monitoring is essential to catch any return of high blood sugar early.
Is remission possible if I’m on insulin?
It’s less common but still possible. People on insulin usually have had diabetes longer and may have more damage to their insulin-producing cells. However, significant weight loss and lifestyle changes have led to remission in some insulin users, especially if they’ve been on it for less than five years. It requires close medical supervision.
How long should I wait after losing weight to check for remission?
Wait at least three months after stopping medication or after reaching your weight goal before testing HbA1c. This gives your body time to stabilize. A single normal reading isn’t enough-you need to see consistent results over time. Doctors recommend testing at least once a year after remission is confirmed.
Can I go back into remission if I lose weight again after relapsing?
Yes. Many people regain weight and see their blood sugar rise again-but if they lose the weight once more, remission is often possible again. The body doesn’t lose its ability to respond to weight loss. Each attempt at remission builds on the last, even if it takes more time or effort.
If you’re thinking about remission, start with your doctor-not a fad diet. The science is clear: weight loss works. But only if it’s done safely, sustainably, and with support.





Kelly McRainey Moore
January 20, 2026 AT 06:38Man, I love how this post breaks it down without fluff. I’ve been in remission for 18 months now-lost 28 lbs, stopped metformin, and honestly? The hardest part wasn’t the diet, it was not feeling guilty when I ate pizza on a Friday night. My doctor says I’m doing great, but I still get my HbA1c checked every six months. Just because I’m off meds doesn’t mean I’m off the hook.
lokesh prasanth
January 21, 2026 AT 06:48weight loss works. fat in liver bad. pancreas wakes up. done. no magic. no cure. just math. calories in vs out. why is this so hard for people to get?
michelle Brownsea
January 23, 2026 AT 05:58Let me just say this: if you're still clinging to the idea that diabetes is 'curable' through 'willpower,' you're not just misinformed-you're dangerously naive. Remission isn't a reward for being 'disciplined'; it's a physiological reset that only works for some, under specific conditions. And yet, the wellness industrial complex turns this into a moral victory lap: 'I lost weight, therefore I'm better than you.' No. You're just lucky. Your pancreas didn't burn out yet. Your insulin resistance wasn't advanced. Your body still had plasticity. Stop glorifying this like it's a virtue. It's biology. Not a merit badge.
And for the love of all that's holy, stop telling people who are on insulin that they 'just need to try harder.' Some of us have been fighting this for 15 years. We've done the keto, the fasting, the 10,000 steps. We've cried in the grocery store because the insulin costs more than rent. And now you want us to feel ashamed because we're not 'in remission'? That's not motivation. That's cruelty dressed up as science.
Roisin Kelly
January 23, 2026 AT 12:23Yeah right. And I'm supposed to believe Big Pharma isn't just letting us think this is real so we stop buying their $500/month drugs? They don't want us cured. They want us 'in remission'-so we keep coming back for 'maintenance' checkups and glucose monitors. It's all a scam. The real cure? Get off the grid. Eat wild plants. Stop using processed salt. They don't want you to know that.
Ashok Sakra
January 25, 2026 AT 03:55why do they make it so hard? i lost 20 lbs and still got diabetes back. i hate this. i just want to eat pizza and not die. why is life like this??
Andrew Rinaldi
January 26, 2026 AT 20:50I appreciate how the article frames remission as a dynamic state-not a finish line. It’s easy to fall into the trap of thinking ‘if I lose the weight, I’m done.’ But the real work begins after the scale stops moving. Maintenance isn’t punishment; it’s stewardship. I’ve seen friends go from remission to relapse and back again, and the ones who succeed long-term aren’t the ones with the strictest diets-they’re the ones with the most compassion for themselves when they slip. That’s the quiet truth no one talks about.
Yuri Hyuga
January 28, 2026 AT 01:35👏 This is exactly the kind of nuanced, science-backed perspective we need more of. Remission isn’t about perfection-it’s about progress. And the fact that even after relapse, you can try again? That’s hope with teeth. I coach people through this every day, and I tell them: your body remembers how to heal. You just have to give it the space to do it. No shame in needing help. No guilt in needing meds. Just consistency. And yes-pizza on Friday is fine, as long as Monday’s breakfast is beans and eggs. 💪
Coral Bosley
January 28, 2026 AT 06:00They call it remission like it’s some kind of victory lap, but let’s be real-this whole thing is just a glorified version of ‘eat less, move more’ wrapped in medical jargon and glossy infographics. They don’t tell you that 80% of people who lose the weight gain it back within two years, and then they get blamed for being ‘lazy’ or ‘lacking discipline.’ Meanwhile, the pharmaceutical companies are still raking in billions from people who ‘relapsed.’ It’s not science-it’s capitalism with a stethoscope.
Gerard Jordan
January 28, 2026 AT 12:37Thanks for sharing this. I’m on insulin and was told remission wasn’t possible for me-until I lost 35 lbs with a low-calorie plan and a support group. My HbA1c is 5.8% now. Still take a tiny bit of metformin. Still get checked every 6 months. Still eat veggies. Still walk after dinner. I didn’t ‘beat’ diabetes. I learned to live with it better. And that’s enough. 🙏