Holiday Diverticulitis Food Swap Guide
- Steamed green beans
- Quinoa
- Broth-based soup
- Fresh fruit (berries)
- Herbal tea
- Deep-fried onion rings
- White bread
- Cream-based soup
- Candied nuts
- Alcoholic cocktails
Quick Takeaways
- Know which holiday foods trigger inflammation and swap them for low‑residue options.
- Plan meals ahead of time; a simple grocery list can keep you on track.
- Stay hydrated, move gently, and keep rescue meds handy.
- Watch for red‑flag symptoms like fever or severe pain - call your doctor early.
- A short checklist can turn a stressful dinner into a manageable event.
Diverticulitis can feel like a party‑crasher when family gatherings roll around. The good news? With a bit of foresight and some practical tricks, you can still enjoy the holidays without a flare‑up.
What Is Diverticulitis?
Diverticulitis is a condition where small pouches called diverticula in the colon become inflamed or infected. Most people develop diverticula after the age of 40, and only a fraction experience painful episodes. The inflammation often flares up when the colon is forced to work harder than usual-think low fiber intake, dehydration, or sudden changes in bowel habits.
Why the Holidays Can Trigger a Flare‑Up
The holiday season packs a perfect storm for the gut: rich, fatty meals, sugary desserts, heavy sauces, and the inevitable toast‑to‑good‑times with alcohol. Those foods are low in fiber and high in residue, which can slow colon movement and increase pressure inside diverticula.
Stress is another hidden culprit. Even the excitement of planning gifts and traveling can raise cortisol levels, nudging the digestive system toward spasms.

Preparing Ahead: Smart Meal Planning
Start your holiday prep a week before the first dinner. Draft a simple menu that balances tradition with low‑residue safety:
- Identify the main dishes you’ll be serving (turkey, ham, roast beef).
- List side dishes that are naturally high in fiber-steamed broccoli, roasted carrots, quinoa.
- Swap starchy mash‑ups for cauliflower mash or sweet‑potato wedges (moderate fiber, easier on the colon).
- Choose a dessert that’s low in added sugars, like baked apples with cinnamon.
- Write a grocery list that includes a fiber supplement (psyllium husk) and a bottle of electrolyte‑rich water.
Having this roadmap means you won’t be scrambling for a suitable snack when the conversation stalls.
Foods to Embrace and Foods to Skip
| Do | Don’t |
|---|---|
| Steamed green beans, carrots, and zucchini | Deep‑fried onion rings, fried chicken skin |
| Quinoa, brown rice, whole‑grain rolls (in moderation) | White bread, buttery rolls, cheese‑filled pastries |
| Broth‑based soups with clear vegetables | Cream‑based soups, chowders, heavy gravies |
| Fresh fruit (apple slices, berries) with no added sugar | Candied nuts, chocolate‑covered treats |
| Herbal teas, water with a splash of lemon | Alcoholic cocktails, sugary sodas |
These swaps keep fiber steady without overloading the colon with tough residue.
Managing Symptoms on the Go
Traveling between relatives can be stressful for anyone, let alone someone dealing with an inflamed colon. Here are quick tactics:
- Hydration: Aim for at least eight 8‑oz glasses of water a day. Carry a reusable bottle and sip continuously.
- Move gently: Short walks after meals help stimulate peristalsis. Even a 5‑minute hallway stroll can make a difference.
- Medication kit: Pack your prescribed antibiotics (if you’re on a course), a mild pain reliever like acetaminophen (avoid NSAIDs unless your doctor says it’s safe), and a fiber supplement.
- Probiotic boost: A daily probiotic containing Lactobacillus and Bifidobacterium strains can help balance gut flora and potentially reduce flare‑up severity.
- Portable snacks: Keep low‑residue snacks in your bag-rice cakes, a small container of unsweetened applesauce, or a handful of plain popcorn.
When to Call Your Doctor
Most mild flare‑ups can be handled at home, but certain signals mean you need professional care right away:
- Fever above 101°F (38.3°C)
- Severe, worsening abdominal pain that doesn’t improve with rest
- Vomiting or inability to keep liquids down for more than 12 hours
- Blood in stool or black, tarry stools
- Sudden swelling or tenderness in the abdomen
If any of these appear, call your gastroenterologist or head to the nearest emergency department. Early treatment can prevent complications like abscesses or perforation.
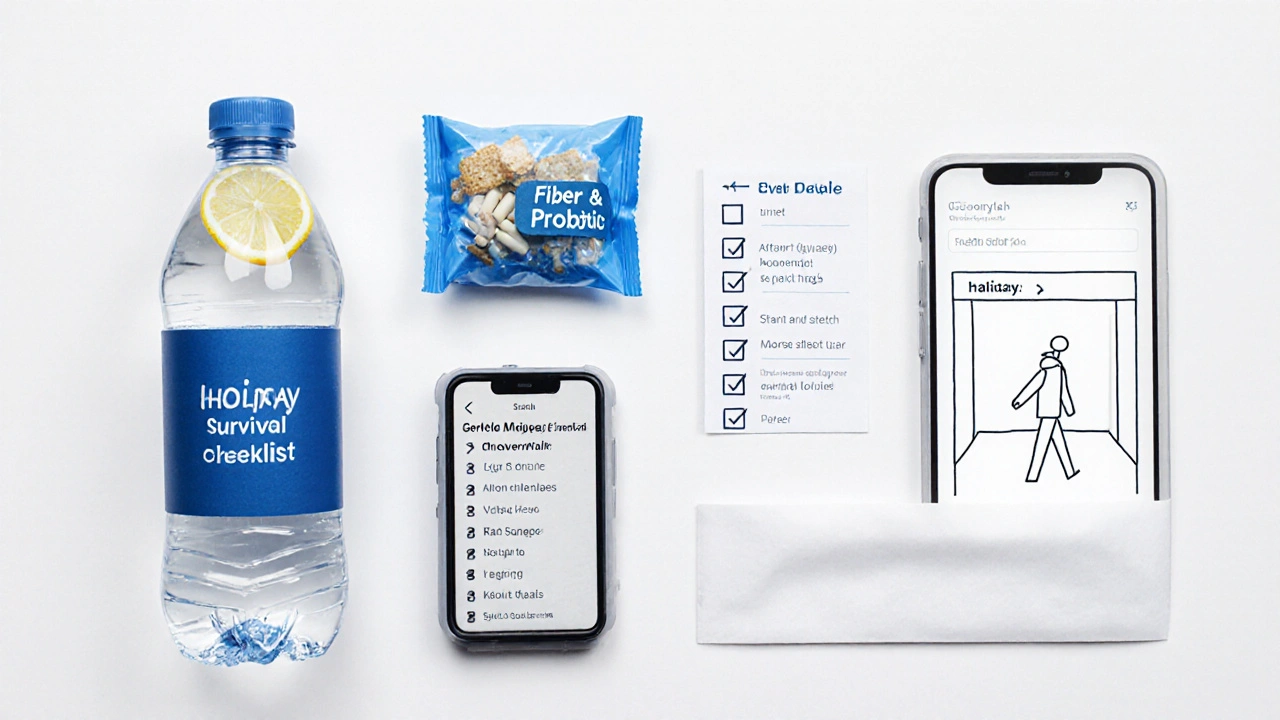
Holiday Survival Checklist
- Confirm your medication schedule with your doctor before the first gathering.
- Print a one‑page food swap guide and place it on the kitchen counter.
- Pack a travel‑size water bottle, fiber supplement packets, and a probiotic pill.
- Set a reminder on your phone to stand up and stretch every 45 minutes.
- Keep a symptom log (pain level, bowel movements, fluid intake) to spot patterns early.
- Designate a “safe snack” spot at each party-maybe a bowl of sliced cucumbers.
- Know the nearest urgent‑care location for each family home you’ll visit.
With these steps, you can focus on the laughter and lights rather than worrying about a sudden stomach ache.
Frequently Asked Questions
Can I enjoy turkey during a diverticulitis flare‑up?
Yes, as long as the turkey is roasted or baked without heavy, fatty gravies. Remove the skin, slice the meat thinly, and pair it with a low‑residue side like steamed carrots.
Is it safe to drink wine or cocktails at holiday parties?
Alcohol can irritate the gut and dehydrate you, increasing the risk of a flare‑up. If you choose to drink, limit yourself to one glass of wine and sip water in between.
How much fiber should I aim for during the holidays?
Aim for 25-30grams of fiber per day, spread across meals. Use a fiber supplement if you’re unsure you’ll hit that target with food alone.
What over‑the‑counter pain relievers are safe?
Acetaminophen (Tylenol) is generally safe. Avoid ibuprofen or naproxen unless your doctor says they won’t worsen inflammation.
Can stress really trigger a diverticulitis flare‑up?
Stress can change gut motility and increase inflammation markers, making a flare‑up more likely. Simple relaxation techniques-deep breathing, short walks, or a few minutes of meditation-can help keep symptoms in check.




Sophie Rabey
October 6, 2025 AT 16:13When you’re juggling the turkey, cranberry sauce, and a low‑residue plan, it feels like a high‑stakes clinical trial. The guide’s swap chart basically functions as a quick‑reference protocol for diverticulitis‑safe nutrition. Just remember, steaming those green beans isn’t just a garnish; it’s a fiber‑sparing maneuver that keeps intraluminal pressure down. And if you ever wonder why the default on the page is “candied nuts,” it’s because the algorithm loves a good challenge.
Bruce Heintz
October 16, 2025 AT 23:49Hey, you’ve got this! Keep the swaps simple, stay hydrated, and don’t let the holiday hype throw you off track 😊. A quick walk after dinner can really help move things along, so consider a post‑meal stroll before the dessert table.
richard king
October 27, 2025 AT 06:25In the theater of the holidays, the gut is the unwatched actor that can seize the spotlight at any moment. Stress whispers like a murmuring philosopher, nudging peristalsis into a chaotic dance. By turning each meal into a mindful ritual, you rewrite the script and keep the colon from demanding an encore.
Dalton Hackett
November 6, 2025 AT 14:01The importance of pre‑planning cannot be overstated when managing diverticulitis during festive gatherings. First, compile a list of low‑residue foods that you are comfortable consuming, such as steamed vegetables, broth‑based soups, and quinoa. Second, communicate your dietary needs to the host well in advance, proposing suitable side‑dish alternatives. Third, keep a supply of fiber supplements and probiotic capsules in a clearly labeled container within your travel bag. Fourth, monitor your fluid intake, aiming for at least eight 8‑oz glasses of water each day, because dehydration is a common trigger. Fifth, schedule brief walks of five to ten minutes after each large meal to stimulate peristalsis. Sixth, avoid alcohol and sugary cocktails, which can both irritate the mucosa and increase inflammatory markers. Seventh, if you must indulge in a richer dish, balance it with an immediate low‑residue side such as a cucumber salad. Keep a symptom diary noting pain levels, bowel movements, and any deviations from your baseline. Review the diary nightly to detect patterns that might necessitate medication adjustments. Carry a compact kit containing acetaminophen, your prescribed antibiotics, and a small packet of psyllium husk. Be prepared to seek medical attention promptly if fever, worsening pain, or vomiting develop. Remember that stress management techniques-deep breathing, brief meditation, or listening to calming music-can lower cortisol and reduce gut motility disturbances. Enlist a family member as a “food‑swap buddy” to help you navigate the buffet line without feeling isolated. Finally, enjoy the company of loved ones; the psychological benefit of social support often outweighs the temporary inconvenience of a modified plate.
William Lawrence
November 16, 2025 AT 21:37Sure, because nothing says holiday cheer like a colon flare‑up.
Grace Shaw
November 27, 2025 AT 05:12It is essential to delineate the parameters of a safe holiday menu with scholarly precision. By adhering to evidence‑based recommendations, one can mitigate the risk of diverticulitis exacerbation whilst still partaking in convivial gatherings. I advise the inclusion of low‑residue vegetables, such as steamed green beans and carrots, as they furnish necessary micronutrients without imposing excessive luminal bulk. Moreover, substituting cream‑based soups with clear broth preparations diminishes the probability of obstructive sequelae. Maintaining adequate hydration-approximately two liters of aqueous fluids per diem-serves to preserve stool softness and promote transit. In addition, a brief ambulatory routine subsequent to each repast facilitates peristaltic activity, thereby reducing intraluminal pressure. Should alarming symptoms arise, including febrile states or persistent abdominal pain, immediate medical consultation is warranted. This methodical approach balances festive enjoyment with gastrointestinal prudence.
Sean Powell
December 7, 2025 AT 12:48Yo fam lets keep it real – swap that greasy drippin’ gravy for a light veggie broth its the move stay chill and your gut will thank u
Henry Clay
December 17, 2025 AT 20:24Look the data is crystal clear people ignore the simple swaps and end up in the ER 🙄 if you want to survive the feast follow the guide no excuses
Isha Khullar
December 28, 2025 AT 04:00The holiday lights glitter but my gut roars like a storm inside, every deep‑fried bite feels like a betrayal, the swap is my only salvation
Lila Tyas
January 7, 2026 AT 11:36Let’s get pumped for a healthy holiday! 🎉 Load up that plate with quinoa, splash on some lemon‑herb broth, and keep the water bottle handy. A quick stretch between courses can be a game‑changer, and don’t forget to celebrate the small wins when you stick to the plan. You’ve got the power to make this season both joyful and gentle on your gut!
Mark Szwarc
January 17, 2026 AT 19:12Pro tip: keep a pocket‑size checklist that lists “green beans, quinoa, broth, fruit” and tick them off as you fill your plate. If a dish looks suspicious – heavy, fried, or cheesy – swap it immediately using the guide’s suggestions. Also, set an alarm on your phone for every 45 minutes to stand up and do a brief walk; it’s amazing how much that helps keep things moving. And remember, acetaminophen is your go‑to pain reliever, but avoid NSAIDs unless your doctor gave the green light.
BLAKE LUND
January 28, 2026 AT 02:48Around the world the holidays look different but the idea stays the same – share food, share love, and keep the gut happy with simple swaps.
Veronica Rodriguez
February 7, 2026 AT 10:24Great reminder to pack a small snack like rice cakes or unsweetened applesauce for travel stops 😊. It’s a lifesaver when the buffet options get limited.
Holly Hayes
February 17, 2026 AT 15:13Honestly, if you cant even read the ingredient list you’re basically signing up for a colon catastrophe, lol.