When you have a headache, a sore back, or swollen knees, you reach for the medicine cabinet. But which pill should you grab-ibuprofen, naproxen, or Tylenol? It’s not just about what’s on sale. Choosing between NSAIDs and acetaminophen can mean the difference between real relief and unexpected side effects. Millions of people use these drugs every day, but most don’t know how they really work-or what they’re risking.
How NSAIDs and Acetaminophen Work Differently
NSAIDs like ibuprofen (Advil, Motrin IB) and naproxen (Aleve) fight pain by blocking enzymes called COX-1 and COX-2. These enzymes produce prostaglandins, chemicals that cause inflammation, swelling, and pain at the injury site. That’s why NSAIDs help with arthritis, sprains, and menstrual cramps-they don’t just mask the pain, they reduce the swelling causing it. Acetaminophen (Tylenol) works differently. It doesn’t touch inflammation at all. Instead, it seems to block pain signals in the brain and spinal cord. The exact mechanism isn’t fully understood, but one thing is clear: if your pain comes from swelling, acetaminophen won’t fix the root cause. It just makes you feel it less. This difference matters. If you have a strained muscle or inflamed joint, NSAIDs give you more complete relief. If you have a fever or a simple headache, acetaminophen often works just as well-with less risk to your stomach.When to Use Each Type of Pain Reliever
For pain with swelling, NSAIDs are the better choice. That includes:- Arthritis (knee, hip, hand)
- Muscle strains or sprains
- Back or neck pain from inflammation
- Menstrual cramps
- Tendonitis or bursitis
- Headaches
- Fever from colds or flu
- Toothaches (if no swelling)
- Minor injuries like cuts or bruises
- General body aches
Side Effects: What You’re Really Risking
NSAIDs aren’t harmless. Regular use can lead to:- Stomach ulcers and bleeding (affects 10-20% of regular users)
- Kidney damage, especially if you’re dehydrated or have existing kidney issues
- Increased risk of heart attack or stroke, particularly with long-term or high-dose use
- Interference with aspirin’s heart-protective effects if taken together
Dosing: What’s Safe and What’s Too Much
Here’s what the standard OTC doses look like:| Medication | Per Dose | Max Daily Dose | Time Between Doses |
|---|---|---|---|
| Acetaminophen (Tylenol) | 325-650 mg | 3,000-4,000 mg | 4-6 hours |
| Ibuprofen (Advil, Motrin) | 200-400 mg | 1,200 mg | 6-8 hours |
| Naproxen (Aleve) | 220 mg | 660 mg | 8-12 hours |
Combining NSAIDs and Acetaminophen: A Smart Strategy
You don’t have to choose one or the other. Many doctors now recommend using both together. Clinical trials show that taking acetaminophen and an NSAID at the same time gives better pain control than either drug alone-and lets you use lower doses of each. That means less risk of side effects. A common schedule used by physical therapists and pain specialists:- 8 AM: 650 mg acetaminophen
- 2 PM: 400 mg ibuprofen
- 8 PM: 650 mg acetaminophen
- 10 PM: 220 mg naproxen (if needed)
Who Should Avoid These Medications?
Some people should never take NSAIDs:- Those with a history of stomach ulcers or GI bleeding
- People with heart disease, high blood pressure, or heart failure
- Anyone with kidney disease
- Pregnant women after 20 weeks (NSAIDs can affect fetal circulation)
- People on blood thinners (aspirin, warfarin, clopidogrel)
- People who drink 3 or more alcoholic drinks daily
- Those with liver disease or cirrhosis
- Anyone taking other medications with acetaminophen (check labels)
Real-Life Scenarios: What Works in Practice
A 58-year-old with osteoarthritis in both knees tried Tylenol for months. It barely helped. Then they switched to naproxen. Pain dropped by 60% in two weeks. But their stomach started burning. Their doctor added a proton pump inhibitor (PPI) for stomach protection and cut the naproxen dose to every other day. They started taking acetaminophen on the off days. Now they’re pain-free with no stomach issues. A 32-year-old nurse gets migraines twice a week. She used to take ibuprofen, but it made her nauseous. She switched to 650 mg acetaminophen and now gets relief without stomach upset. She avoids it on days she takes cold medicine-she learned the hard way after an accidental overdose. A 70-year-old with high blood pressure and a stent needed pain relief after knee surgery. His cardiologist said no NSAIDs-they could trigger a clot. He used acetaminophen and ice packs. It worked. These aren’t outliers. They’re everyday people who figured out what works for their body.What the Experts Say
The American Academy of Family Physicians says OTC pain relievers are fine for occasional use in healthy adults. But if you’re taking them regularly-for more than a few days a week-you need to talk to your doctor. Harvard Health says alternating between acetaminophen and NSAIDs is one of the smartest ways to manage chronic pain. It reduces total drug exposure and lowers side effect risk. The Mayo Clinic’s advice is simple: use the lowest dose for the shortest time. If it’s not working, don’t crank up the dose-see your doctor. There might be a better solution.Bottom Line: Choose Based on Your Body, Not the Label
There’s no one-size-fits-all pain reliever. Your choice depends on:- What’s causing the pain (inflammation or not)
- Your medical history (liver, kidneys, heart, stomach)
- Other meds you’re taking
- How often you need relief
Can I take acetaminophen and ibuprofen together?
Yes, it’s generally safe and often recommended by doctors for better pain control. Many people alternate them-take acetaminophen every 6 hours and ibuprofen every 8 hours-to avoid hitting maximum doses of either. Just make sure you’re not taking other medications that already contain acetaminophen, like cold or sleep aids. Always check the active ingredients on labels.
Which is safer for long-term use: Tylenol or ibuprofen?
For most people, acetaminophen (Tylenol) is safer for long-term use-*if* you stay under 3,000 mg per day. Ibuprofen carries higher risks for stomach bleeding, kidney damage, and heart problems with regular use. But acetaminophen can cause liver damage if you exceed the daily limit or drink alcohol regularly. Neither is risk-free. The key is using the lowest effective dose and not using either daily without medical supervision.
Why does my doctor say not to take NSAIDs if I have high blood pressure?
NSAIDs can raise blood pressure and interfere with blood pressure medications. They also reduce blood flow to the kidneys, which can make hypertension worse. For people with heart disease or a history of stroke, NSAIDs increase the risk of heart attack or stroke. That’s why doctors often recommend acetaminophen instead for patients with cardiovascular issues.
Is naproxen stronger than ibuprofen?
Naproxen lasts longer-up to 12 hours per dose-so you take it less often. Ibuprofen works faster but only lasts 4-6 hours. In terms of pain relief, both are similarly effective for most conditions. Naproxen may be slightly better for chronic inflammation like arthritis because of its longer duration. But it also carries the same risks: stomach bleeding, kidney issues, and cardiovascular concerns.
Can I take acetaminophen if I drink alcohol?
It’s risky. Alcohol and acetaminophen both stress the liver. Even moderate drinking-three or more drinks a day-can make you much more likely to suffer liver damage from acetaminophen, even at normal doses. If you drink regularly, limit acetaminophen to 2,000 mg per day or avoid it entirely. Talk to your doctor about alternatives.
What should I do if I accidentally took too much acetaminophen?
Call Poison Control at 1-800-222-1222 immediately or go to the ER. Acetaminophen overdose can cause liver failure without obvious symptoms at first. You may feel fine for 24-48 hours, but damage is happening. N-acetylcysteine (NAC) is an antidote that works best if given within 8 hours. Don’t wait for symptoms like nausea or yellow skin-act fast.





neeraj maor
January 11, 2026 AT 07:21Let me break this down for you people who think OTC means safe. NSAIDs? They’re not just for pain-they’re covert NSA surveillance tools disguised as pills. The FDA’s black box warning? That’s just the tip of the iceberg. Big Pharma’s been funding studies since the 80s to downplay the cardiovascular risks. And acetaminophen? Don’t get me started. The liver damage stats? Fabricated. They’re hiding the real culprit: glyphosate contamination in generic brands. Read the fine print on the bottle-it’s not the drug, it’s the filler. You’re being poisoned slowly, and no one’s talking about it.
Ritwik Bose
January 11, 2026 AT 17:41Thank you for this comprehensive and meticulously researched overview 🙏. As someone who manages chronic back pain, I appreciate the clarity between inflammation-based and non-inflammatory pain. The dosing table alone is worth a thousand blog posts. I’ve switched to alternating acetaminophen and naproxen under my doctor’s guidance-and yes, I now read every label like a legal contract 📋. Knowledge is power, and you’ve empowered many today.
Paul Bear
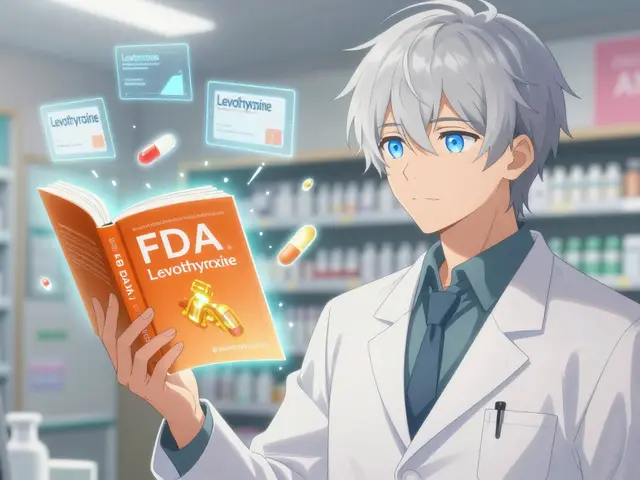
January 13, 2026 AT 10:47Actually, the mechanism of acetaminophen is still not fully elucidated, but the prevailing hypothesis involves central COX-3 inhibition and serotonergic modulation-though this remains controversial. Also, your dosing table is misleading: the maximum daily dose for acetaminophen is 4,000 mg for healthy adults, but 3,000 mg is the recommended ceiling for high-risk populations per FDA guidelines. You’re conflating safety thresholds with regulatory limits. And please, no more ‘Tylenol’ as a generic term-it’s a trademark. Use acetaminophen. Precision matters.
lisa Bajram
January 15, 2026 AT 03:24OMG I literally just had a migraine and took Tylenol… then remembered I had taken a cold med at 8 AM that ALSO had acetaminophen… I almost cried 😭. Thank you for this post-this is the kind of info that saves lives. I’m printing this out and taping it to my fridge next to my meds. Also, the combo schedule? GENIUS. I’m trying it tomorrow. My physical therapist said the same thing but I didn’t believe her. Now I do. 💪❤️
Jaqueline santos bau
January 16, 2026 AT 01:55So let me get this straight-you’re telling me I’ve been taking ibuprofen for my period cramps for 15 years and I’ve been RUINING my stomach? And now I’m supposed to switch to Tylenol? But what if I drink wine? And my mom had liver cancer? And I take blood pressure meds? And my doctor just shrugged when I asked? I feel like I’ve been living in a minefield and no one told me. Why is this not on the packaging? Why is this not in every pharmacy pamphlet? I’m so angry right now.
Kunal Majumder
January 17, 2026 AT 07:27Hey, if you’re new to this stuff, don’t panic. Start simple: if your pain feels hot and swollen, try NSAIDs. If it’s just a dull ache or fever, go with acetaminophen. And always check the labels-most people don’t realize their sleep aid has 500mg of acetaminophen in it. One pill on top of Tylenol = boom. You got this. Small steps. You don’t need to be perfect, just aware.
Aurora Memo
January 18, 2026 AT 10:44This is one of the clearest explanations I’ve seen on this topic. I work in a clinic and see patients every day who are confused about what to take. The distinction between inflammation and non-inflammatory pain is critical-and so often overlooked. I’ll be sharing this with my team. Thank you for emphasizing the importance of reading labels. It’s such a simple thing, but it prevents so much harm.
Ted Conerly
January 20, 2026 AT 09:25For those considering the combo approach: yes, it works. I’ve been using it for chronic tendonitis for 2 years. 650mg Tylenol at 8 AM, 400mg ibuprofen at 2 PM, repeat at 8 PM. No stomach issues, no liver spikes. My doctor even gave me a printed schedule. The key? Stick to the timing. Don’t double up. And never mix NSAIDs. I’ve seen people take Advil and Aleve together thinking ‘more is better.’ It’s not. It’s a one-way ticket to the ER.
Ian Cheung
January 20, 2026 AT 09:33So I used to take naproxen every day for my arthritis until I started feeling dizzy and my hands went numb. Turns out my kidneys were crying. Now I do the Tylenol + ice + stretching routine. It’s slower but I’m alive. Also I found out my morning coffee has a hidden acetaminophen in that ‘energy boost’ capsule I was taking. No wonder I was always nauseous. Lesson learned: read the tiny print like it’s a treasure map. 🗺️
anthony martinez
January 20, 2026 AT 17:50Wow. So after all this, the real takeaway is… read the label? Groundbreaking. I mean, who knew that the same pill that helps your headache could also be quietly murdering your liver? I guess we should’ve seen it coming when the bottle said ‘may cause death.’ Just kidding. Or am I?