CKD Stage to RCC Risk Calculator
Chronic Kidney Disease Stage Information
Select your current CKD stage to see associated risk level for advanced renal cell carcinoma:
Risk Assessment Results
Estimated Risk Multiplier:
Time to Cancer Diagnosis (Median):
Advanced Cancer Detection Rate:
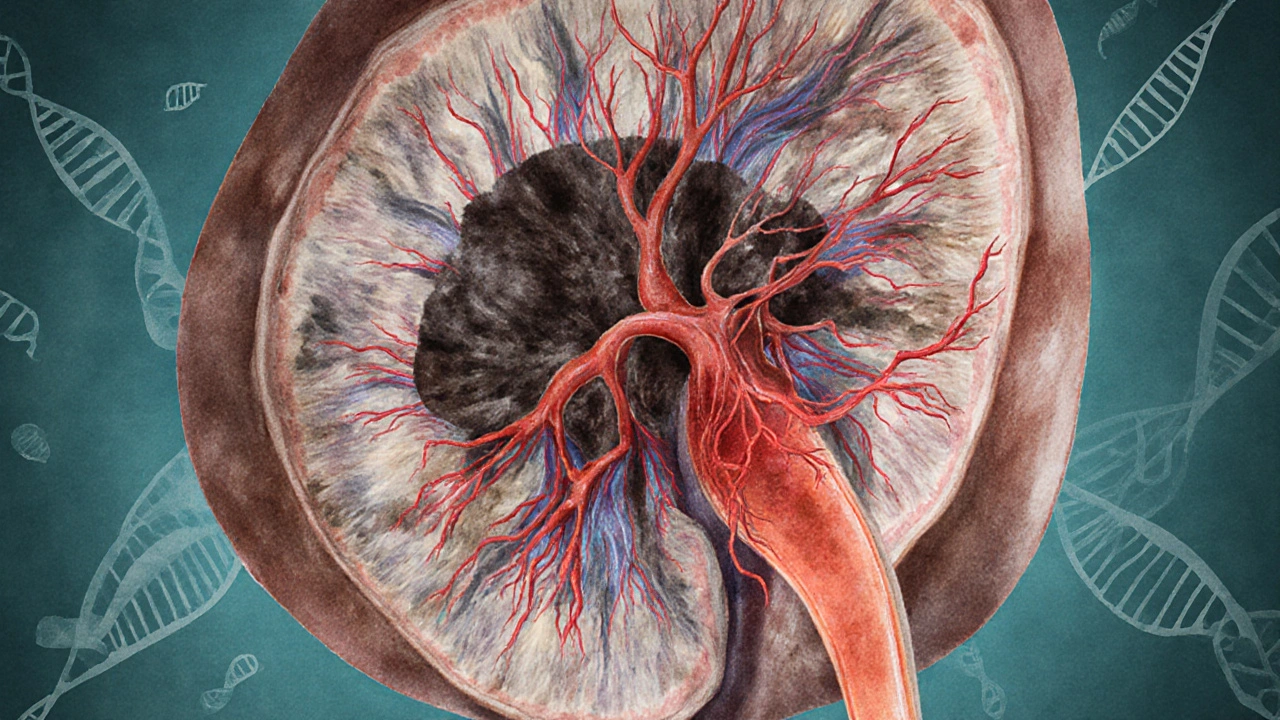
When Chronic Kidney Disease is described as a gradual loss of kidney function, most people picture fatigue, swelling, or the need for dialysis. A long‑term decline in glomerular filtration, often measured by eGFR, can set the stage for other serious problems. Understanding chronic kidney disease is the first step toward grasping why it matters for cancer, especially the aggressive form of kidney cancer known as advanced renal cell carcinoma.
What Is Chronic Kidney Disease?
Glomerular Filtration Rate (GFR) is the gold‑standard metric doctors use to stage CKD. A normal GFR is above 90mL/min/1.73m²; values drop as the disease progresses. Stages1‑5 reflect increasing severity, with stage5-also called end‑stage renal disease (ESRD)-requiring dialysis or transplantation.
- Stage1: GFR ≥90, kidney damage present
- Stage2: GFR 60‑89
- Stage3a: GFR 45‑59
- Stage3b: GFR 30‑44
- Stage4: GFR 15‑29
- Stage5: GFR <15 (ESRD)
Renal Cell Carcinoma at a Glance
Renal Cell Carcinoma (RCC) accounts for about 90% of kidney cancers. When the tumor spreads beyond the kidney-invading the veins, lungs, or bones-it is classified as Advanced Renal Cell Carcinoma. Advanced RCC carries a five‑year survival rate of roughly 12‑15%, compared with >90% for localized disease.
Why CKD Raises the Risk of Advanced RCC
Several biological pathways link a chronically damaged kidney to a more aggressive cancer:
- VHL Gene mutations are common in both CKD‑related cystic disease and sporadic RCC. Loss of VHL function triggers unchecked Angiogenesis, feeding tumor growth.
- Uremic toxins accumulate as GFR falls, creating a pro‑inflammatory environment that stimulates cytokines such as IL‑6 and TNF‑α, which in turn promote tumor cell proliferation.
- Patients with CKD often have hypertension, diabetes, and smoking history-classic RCC risk factors. The combination amplifies DNA damage and oxidative stress.
Clinical Evidence of the Link
A 2023 multicenter cohort of 12,000 CKD patients showed a 2.7‑fold higher incidence of RCC compared with age‑matched controls. Notably, those who progressed to stage4 or5 had a median time to cancer diagnosis of 4.2years, and 68% of those cancers were already advanced at detection.
Another prospective study published in the Journal of Oncology (2024) tracked biomarkers like VEGF and CA‑IX. Elevated levels correlated with both lower eGFR and higher tumor grade, reinforcing the angiogenesis connection.
Screening Recommendations for High‑Risk CKD Patients
Guidelines now suggest more aggressive surveillance when CKD reaches stage3b or higher. A practical algorithm:
- Annual renal ultrasound for stages3b‑5, regardless of symptoms.
- If a solid mass >1cm is seen, proceed to contrast‑enhanced CT or MRI (unless contraindicated by contrast allergy or severe renal impairment).
- Check serum biomarkers (VEGF, CA‑IX) when imaging is equivocal.
- Refer to a multidisciplinary oncology team promptly if any suspicious finding emerges.
Treatment Strategies When CKD and Advanced RCC Co‑exist
Therapeutic choices must balance kidney function with cancer control:
- Nephrectomy (partial or radical) remains a cornerstone, but surgeons now prefer minimally invasive approaches to preserve residual renal mass.
- Targeted Therapy (e.g., sunitinib, pazopanib) requires dose adjustments for eGFR <30mL/min. Therapeutic drug monitoring can prevent toxicity.
- Immunotherapy with PD‑1/PD‑L1 inhibitors (nivolumab, pembrolizumab) shows promising response rates even in low‑GFR patients, though clinicians watch for immune‑related nephritis.
- Combination regimens (e.g., axitinib+pembrolizumab) have become first‑line for many advanced RCC cases; phase‑III trials (2025) report median progression‑free survival of 15.2months in CKD stage3‑4 cohorts.
Supportive care-managing anemia, electrolyte balance, and nutritional status-directly influences treatment tolerance and quality of life.

Prognostic Factors Specific to CKD‑Associated RCC
Beyond the usual TNM staging, three CKD‑related variables predict outcome:
| Feature | Risk Increase | Typical Management |
|---|---|---|
| eGFR <30mL/min | Hazard Ratio 1.8 | Reduced drug dose, close labs |
| Proteinuria >1g/day | Hazard Ratio 1.5 | ACE‑I/ARB therapy, nephrology consult |
| Persistent hyperphosphatemia | Hazard Ratio 1.4 | Dietary phosphate binders |
These markers help clinicians decide whether to pursue aggressive systemic therapy or focus on palliation.
Future Directions and Ongoing Research
Researchers are exploring whether early use of SGLT2 inhibitors-a class of diabetes drugs that also slow CKD progression-might indirectly lower RCC risk by reducing oxidative stress. A Phase‑II trial (2025) enrolling 300 CKD stage3 patients reported a 22% drop in circulating VEGF after a year of empagliflozin therapy.
Another exciting avenue is the use of liquid biopsies (circulating tumor DNA) to catch RCC before a mass becomes radiologically visible, especially useful for patients whose kidneys cannot tolerate contrast agents.
Key Takeaways
- CKD creates a pro‑inflammatory, pro‑angiogenic environment that accelerates RCC development and progression.
- Stage3b or higher CKD warrants annual imaging and biomarker surveillance.
- Treatment must be customized: dose‑adjusted targeted agents, careful immunotherapy monitoring, and kidney‑preserving surgery.
- Prognosis depends on both cancer stage and renal function; low eGFR, heavy proteinuria, and hyperphosphatemia worsen outcomes.
- Emerging therapies-including SGLT2 inhibitors and liquid biopsies-could change the landscape in the next few years.
Frequently Asked Questions
Does having CKD automatically mean I will develop kidney cancer?
No. CKD raises the risk, especially at later stages, but most people with CKD never get cancer. Regular monitoring helps catch any problem early.
Can I receive immunotherapy if my kidneys are failing?
Yes, but doctors will start at a lower dose and watch kidney labs closely. Some patients develop immune‑related nephritis, which is treatable if caught early.
How often should I get a kidney ultrasound?
For CKD stages3b‑5, annual imaging is recommended. If you have additional risk factors-smoking, family history of RCC-your doctor may suggest every six months.
Are there lifestyle changes that lower my combined risk?
Control blood pressure and blood sugar, quit smoking, stay active, and maintain a healthy weight. A low‑salt, plant‑rich diet can also reduce inflammation and proteinuria.
What new treatments should I watch for?
SGLT2 inhibitors for CKD, next‑generation checkpoint inhibitors, and circulating tumor DNA tests are in late‑stage trials and may become standard within the next few years.





Dawn Midnight
October 9, 2025 AT 14:56Monitoring GFR trends is essential for managing CKD patients at risk for RCC.
frank hofman
October 15, 2025 AT 01:26I’m not sold on these shiny calculators – they sound fancy but they don’t replace a real doc’s judgement 😂.
Yeah, numbers can guide you, but they’re not the be‑all and end‑all.
Plus, the interface looks like it was made in 1999, lol.
Dannii Willis
October 20, 2025 AT 11:56Interesting overview! The risk stratification based on CKD stage is a solid start, and I appreciate the clear visual layout. It’s helpful for both patients and clinicians to see where they stand without getting bogged down in jargon.
Robyn Du Plooy
October 25, 2025 AT 22:26The integration of eGFR thresholds with oncogenic pathway markers like VEGF and CA‑IX adds a mechanistic layer to the risk model.
From a nephrology‑oncology standpoint, preserving residual renal function while targeting angiogenic drivers is a nuanced balancing act.
Boyd Mardis
October 31, 2025 AT 07:56Let’s be real – the drama of a cancer diagnosis paired with shrinking kidney function is a nightmare scenario, but the data here give us a fighting chance to intervene early.
ayan majumdar
November 5, 2025 AT 18:26i get the point but i think we should also keep it simple for patients they need clear steps not a maze of numbers
Johnpaul Chukwuebuka
November 11, 2025 AT 04:56Stay positive! Knowing your CKD stage empowers you to take proactive steps, and early detection of RCC can dramatically improve outcomes.
Xavier Hernandez
November 16, 2025 AT 15:26It’s morally reprehensible to let a system that could flag high‑risk patients sit idle while profit‑driven motives dictate care.
Zach Yeager
November 22, 2025 AT 01:56We must protect our national health standards and ensure every American gets the best screening regardless of socioeconomic status.
Angel Gallegos
November 27, 2025 AT 12:26The tool is a textbook example of over‑engineering; it pretends to be cutting‑edge while offering nothing beyond what a seasoned nephrologist already knows.
ANTHONY COOK
December 2, 2025 AT 22:56Data shows that ignoring nuanced risk calculators can lead to missed early RCC diagnoses 😑. It’s a cold, analytical fact: utility matters more than flash.
Sarah Aderholdt
December 8, 2025 AT 09:26Balancing cultural health beliefs with evidence‑based screening can bridge gaps in patient adherence, especially when CKD and RCC intersect.
Phoebe Chico
December 13, 2025 AT 19:56Our nation’s future depends on protecting every citizen’s kidneys and kidneys protect the nation’s strength – let’s not be complacent.
Larry Douglas
December 19, 2025 AT 06:26The relationship between chronic kidney disease and advanced renal cell carcinoma is a multifaceted clinical challenge that warrants comprehensive discussion. First, the pathophysiological mechanisms linking reduced glomerular filtration rate to oncogenic transformation involve chronic inflammation, oxidative stress, and dysregulated angiogenic pathways. Second, epidemiological data consistently demonstrate an elevated incidence of RCC among patients with stage 3 and higher CKD, suggesting a dose‑response relationship. Third, diagnostic imaging in this population is complicated by impaired renal clearance of contrast agents, necessitating alternative modalities such as non‑contrast MRI or contrast‑enhanced ultrasound. Fourth, therapeutic decision‑making must balance oncologic efficacy with preservation of residual renal function; dose adjustments for tyrosine kinase inhibitors and careful selection of nephrectomy candidates are paramount. Fifth, interdisciplinary collaboration between nephrologists, oncologists, and radiologists improves risk stratification and patient outcomes. Sixth, emerging biomarkers, including circulating VEGF and tissue carbonic anhydrase IX, hold promise for early detection but require validation in CKD cohorts. Seventh, patient education regarding the significance of regular monitoring and lifestyle modifications can mitigate progression of both diseases. Eighth, health‑policy implications arise as insurers and healthcare systems must consider coverage for advanced screening tools in high‑risk CKD populations. Ninth, future research directions should explore the impact of novel immunotherapeutic agents on renal function and long‑term survivorship. Tenth, clinicians should remain vigilant for atypical presentations of RCC, such as hematuria or flank pain, which may be masked by CKD symptomatology. Eleventh, the integration of electronic health record alerts based on GFR trends could facilitate timely referrals to oncology services. Twelfth, survivorship care plans must incorporate renal monitoring to detect treatment‑related nephrotoxicity. Thirteenth, the psychosocial burden of dual diagnoses underscores the need for supportive counseling services. Fourteenth, cost‑effectiveness analyses are essential to justify widespread implementation of risk calculators in routine practice. Finally, a patient‑centered approach that respects individual values while leveraging evidence‑based risk assessment will ultimately improve both renal and oncologic outcomes.
Michael Stevens
December 24, 2025 AT 16:56Great summary! I’ll share this with my team so we can incorporate these points into our clinic workflow.
Ann Campanella
December 30, 2025 AT 03:26Honestly, this calculator feels like an overhyped gimmick that anyone can ignore.
Desiree Tan
January 4, 2026 AT 13:56Don’t dismiss it outright – even a modest tool can save a life when used correctly.