One wrong dose of IV insulin can kill a patient. Not in a few days. Not after complications. Sometimes within minutes. That’s why hospitals don’t just rely on one nurse to check it. They require two. This isn’t bureaucracy. It’s survival.
What Makes a Medication High-Risk?
Not all medications are created equal. A typo on an aspirin prescription might cause a stomachache. A typo on an IV heparin order can trigger uncontrollable bleeding. High-risk medications are those where even a small mistake-wrong dose, wrong route, wrong patient-can lead to death or permanent injury. The Institute for Safe Medication Practices (ISMP) has been tracking these for over 20 years. Their list isn’t arbitrary. It’s built on real data: which drugs have caused the most harm when given incorrectly. The top offenders? IV opioids, insulin (all types), heparin (especially IV), chemotherapy agents, and concentrated potassium chloride. These aren’t rare drugs. They’re used every day in hospitals, ERs, and ICUs. And they’re unforgiving. A child given a full adult dose of morphine through an IV? Respiratory arrest. A diabetic given 10 units instead of 1? Seizure, coma, brain damage. A patient getting heparin at 10x the intended rate? Internal bleeding. These aren’t hypotheticals. They’ve happened. And they keep happening-because humans make mistakes.Why Two People Must Check It
The standard medication check? One nurse reads the label. One nurse pulls the vial. One nurse pushes the button. That’s not enough for high-risk meds. Independent double checking means two qualified professionals verify the medication separately-before it’s given. Not one person checking while the other watches. Not a pharmacist confirming what a nurse already did. Two people do the math, read the label, confirm the patient, and sign off-without seeing each other’s work. Why? Because confirmation bias is real. If you see someone else already checked it, you’re more likely to nod along. But if you’re the second person and you’re forced to start from scratch, you might catch the 10x overdose the first person missed. That’s the whole point. The Joint Commission requires this. So does the Department of Veterans Affairs. So do most major hospital systems. The rule is simple: if it’s on the high-alert list, two sets of eyes must sign off. No exceptions.Which Medications Need This Level of Scrutiny?
Here’s what actually triggers the double-check requirement in most U.S. hospitals today:- IV insulin-even a 0.1-unit error can crash blood sugar dangerously
- IV opioids (morphine, fentanyl, hydromorphone)-especially for epidural or intrathecal use
- IV heparin and low-molecular-weight heparin (like enoxaparin) in high doses
- Chemotherapy drugs (doxorubicin, paclitaxel, cisplatin)-narrow therapeutic window, high toxicity
- Concentrated potassium chloride (KCl)-one vial in an IV bag can stop a heart
- Calcium channel blockers and beta blockers given IV
- Total parenteral nutrition (TPN)-complex mixtures, high risk of electrolyte imbalance
- Neonatal and pediatric cardiac medications-tiny bodies, tiny margins for error

How the Double Check Actually Works
It’s not just about reading the label. It’s a full audit. The two people must verify the Nine Rights:- Right patient (two identifiers: name + DOB)
- Right drug (name, strength, form)
- Right dose (calculated and re-calculated)
- Right route (IV, IM, subcutaneous-no mixing them up)
- Right time (is this dose due now? Is it overlapping with another?)
- Right documentation (is it recorded before giving?)
- Right reason (why is this being given? Is it still needed?)
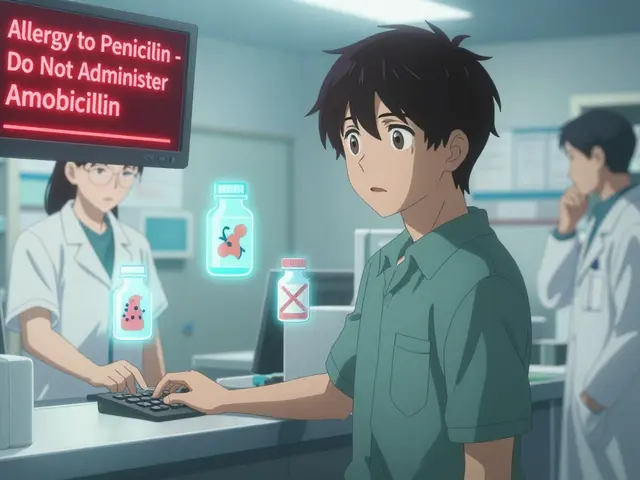
- Right response (has the patient had a reaction before?)
- Right to refuse (has the patient been informed and agreed?)
- Confirm patient identity with two identifiers
- Verify the drug name, dose, volume, and infusion rate
- Check expiration dates and physical condition of the vial
- Confirm the patient understands the treatment
- Sign off on the chart together
The Problem with Double Checks
Here’s the uncomfortable truth: double checks don’t always work. A 2022 ISMP survey found that 68% of nurses admitted skipping required double checks during busy shifts. Why? Forty-two percent said there was simply no second person available. Others said it took too long. Some said they trusted their own judgment too much. And here’s the bigger issue: if you’re doing double checks for everything, you start to tune out. It becomes a checkbox. You’re checking because you have to, not because you’re thinking. That’s when errors slip through. The ISMP now says bluntly: “Fewer independent double checks, strategically placed, are more effective than an overabundance.” In other words, don’t double-check everything. Double-check only what will actually save a life.
What’s Replacing Manual Checks?
Technology is stepping in-not to replace humans, but to support them. Barcode scanning at the bedside is now standard in most hospitals. Before giving any medication, the nurse scans the patient’s wristband and the drug’s barcode. The system says: “This patient isn’t supposed to get this drug.” Or: “This dose exceeds the maximum safe limit.” That catches errors before the nurse even picks up the vial. Smart infusion pumps can be programmed with drug libraries. If you try to set a morphine drip at 20 mg/hour, the pump will flash a warning. It won’t let you proceed. The Veterans Health Administration is rolling out full barcode and smart pump integration by the end of 2024. They’re not eliminating double checks-they’re making them smarter. For example, a nurse still does a manual double check for a new chemotherapy regimen, but the barcode system already confirmed the drug, dose, and patient. The human check now focuses on the harder stuff: is the patient stable? Are the labs okay? Is this still the right plan?What’s the Bottom Line?
High-risk medications aren’t the enemy. They’re necessary. But they’re dangerous. And humans are fallible. The solution isn’t more rules. It’s smarter rules. Focus double checks on the drugs that kill fastest. Use technology to catch the easy mistakes. Train staff not just to check, but to think. And never, ever let convenience override safety. If you work in a hospital, you’ve probably seen someone rush through a double check. Maybe you’ve done it yourself. But when it comes to IV insulin, heparin, or chemo, there’s no such thing as a “quick check.” One mistake. One skipped step. One tired nurse. One missed label. That’s all it takes. Don’t let it be yours.What medications require a double check in hospitals?
Medications that require a double check include IV insulin, IV opioids (like morphine or fentanyl), IV heparin, concentrated potassium chloride, chemotherapy drugs, and total parenteral nutrition (TPN). These are classified as high-alert medications because even small errors can cause death or serious harm. Hospitals also often require double checks for IV calcium channel blockers, beta blockers, and all cardiac medications given to children or newborns.
Who can perform a double check?
Only licensed healthcare professionals who are trained and authorized to administer medications can perform a double check. This typically includes registered nurses, pharmacists, physicians, nurse practitioners, and physician assistants. Unlicensed staff, such as medical assistants or unit clerks, are not permitted to serve as the second checker. The second person must be qualified to independently verify the medication and recognize potential errors.
Is a double check always effective?
No. Studies show that double checks can fail when they’re done too often, rushed, or performed by staff under pressure. Nurses often skip them during busy shifts due to lack of time or staff. The key is not to use double checks for every medication, but to reserve them for the highest-risk drugs. When combined with barcode scanning and smart infusion pumps, manual double checks become far more effective.
Can technology replace the need for double checks?
Technology doesn’t replace double checks-it enhances them. Barcode scanning prevents the wrong drug or patient from being selected. Smart pumps block unsafe doses. But for complex tasks like preparing chemotherapy or adjusting high-risk infusions, human judgment is still essential. The best systems use technology to handle routine verification and free up staff to focus on the nuanced decisions that machines can’t make.
Why is independent double checking important?
Independent double checking means the second person verifies the medication without seeing the first person’s work. This prevents confirmation bias, where the second person just agrees with the first instead of truly checking. It’s the only way to catch mistakes the first person missed-like misreading a label, miscalculating a dose, or confusing similar-looking drugs. Without independence, the second check is just a formality.
Are double checks required by law?
Yes. The Joint Commission requires hospitals to identify high-alert medications and implement safety procedures for them, including independent double checks where appropriate. The Department of Veterans Affairs and many state pharmacy boards have similar mandates. While the exact list of drugs varies by facility, the requirement to have a written policy and follow it is non-negotiable.





Spencer Garcia
December 23, 2025 AT 16:56Double checks aren't just policy-they're the last line of defense when your brain is fried at 3 AM. I've seen a 10x insulin dose get caught because the second nurse actually read the vial. No drama. Just quiet, focused verification. That’s how we survive.
Abby Polhill
December 24, 2025 AT 07:11Let’s be real-chemo double-checks are a whole other level. You got two RNs standing there like forensic accountants, cross-referencing the protocol, the barcode, the patient’s labs, the damn infusion pump settings. If you’re not sweating by the end, you’re not doing it right. And yeah, the smart pumps help, but they don’t replace the human audit. Not yet.
Lindsey Kidd
December 25, 2025 AT 00:14My favorite part? When the second checker says, ‘Wait… that’s not the right concentration.’ 🙌 We’ve all been there. One tiny typo, one misread decimal, and boom-life or death. Thank god for the second pair of eyes. 🤝
Austin LeBlanc
December 25, 2025 AT 18:21Ugh, I hate when nurses skip the double check because they’re ‘too busy.’ You think you’re saving time? You’re just gambling with someone’s life. And don’t even get me started on the ones who ‘trust their gut.’ Your gut doesn’t have a license to kill.
Aurora Daisy
December 27, 2025 AT 04:30Of course Americans need two people to check a syringe. In the UK, we just train our nurses properly and trust them. But hey, if you need a safety net because your system’s broken, I guess that’s your problem.
Isaac Bonillo Alcaina
December 27, 2025 AT 21:10Correction: The Nine Rights include ‘Right route’ and ‘Right reason,’ but the original ISMP framework lists ‘Right documentation’ as part of the ‘Right time’ and ‘Right patient’ validation process. You’re mixing clinical practice with bureaucratic checklist culture. Precision matters.
Dan Gaytan
December 28, 2025 AT 18:05Just had a shift where a new grad almost gave KCl via IV push instead of dilution. Second nurse caught it. We all had a moment of silence. Then coffee. Then we hugged. That’s the real work. Not the paperwork. The human moment after the close call.
Usha Sundar
December 29, 2025 AT 10:58My cousin died from a heparin error. No double check. Just one tired nurse. Don’t make my family’s pain your routine.
Harsh Khandelwal
December 30, 2025 AT 05:03They say ‘two checks save lives’ but who’s really behind this? Pharma companies. More checks = more paperwork = more billing codes. They don’t care if you live or die-they care if the audit trail is perfect. Just saying.
Andy Grace
December 30, 2025 AT 13:55I worked in a rural ER where we didn’t always have two RNs on shift. We used barcode scanning and smart pumps as our backup. The double check became a mental ritual, not a physical one. Sometimes, tech isn’t the enemy-it’s the bridge.
Bret Freeman
January 1, 2026 AT 03:32It’s not about the drugs. It’s about the culture. If your hospital lets nurses rush through double checks because they’re ‘too busy,’ then you’re not a healthcare system-you’re a death sentence with a clipboard. And the people who skip them? They’re not heroes. They’re negligent.
Blow Job
January 1, 2026 AT 11:06Just had a new nurse ask me why we double-check insulin. I told her: ‘Imagine your kid’s heart stopping because someone misread a decimal. Now go do the check like your life depends on it-because someone else’s does.’ She didn’t skip one after that.
Delilah Rose
January 2, 2026 AT 13:04Look, I get why people think double checks are bureaucratic nonsense. I used to be one of them-until I saw a pharmacist catch a 1000-unit insulin vial labeled as 100 units because the barcode was smudged and the nurse assumed it was the same as last time. That’s not paranoia. That’s pattern recognition. And yeah, it takes time. But think about this: how many lives are you willing to risk to save five minutes? I’ve worked nights where I was so tired I could barely stand, and I still made sure the second person did their own math. Because if I’m too exhausted to trust myself, I need someone else to be the anchor. It’s not about blame. It’s about humility. We’re not gods. We’re humans with trembling hands and fading focus. The system exists because we’re all capable of screwing up-even when we mean well. And honestly? I’d rather be the one who slowed down and asked, ‘Wait, did we really check this?’ than the one who said, ‘I’m sure it’s fine,’ and watched someone die because I was too proud to admit I might be wrong. That’s not bureaucracy. That’s love in scrubs.